Why CGMs Aren’t Just for Diabetes Anymore (and How to Use Them Right)
A continuous glucose monitor (CGM) is a small, wearable sensor that measures glucose levels in real time. Instead of getting a single fasting glucose reading at the doctor’s office, a CGM creates a continuous picture—tracking rises, dips, and patterns throughout the day and night.
Originally designed for people with insulin-dependent diabetes, CGMs have now caught the attention of health-conscious consumers, athletes, and clinicians interested in optimizing metabolic health.
The shift? Moving from a reactive medical tool to a proactive lifestyle and prevention tool.
From Diabetes Management to Mainstream Use (and the Debate)
CGMs were originally introduced in the early 2000s to help people with type 1 diabetes — and later type 2 diabetes — manage insulin dosing and prevent dangerous highs and lows. By offering real-time feedback, these devices transformed diabetes management.
Today, two main players dominate the market:
- Freestyle Libre
- Dexcom
Dexcom introduced Stelo, the first over-the-counter (OTC) continuous glucose monitor cleared by the FDA in March 2024 for non‑insulin using adults — both those with type 2 diabetes and people without diabetes.
Abbott followed with Lingo (for wellness-focused users) and Libre Rio (for adults with type 2 diabetes not on insulin), both cleared by the FDA for OTC use in June 2024.
How they work:
Each device typically lasts about 14 days (the new OTC devices are approved for 15 days) and connects to your phone for easy tracking. Some versions allow your clinician to view your data on a secure dashboard, and integrations — like with Stelo or Oura Ring — can overlay glucose with other biometric data such as sleep and recovery. This opens the door to deeper, more holistic health insights.
The controversy:
Some experts argue that CGMs risk “medicalizing” healthy people, creating unnecessary anxiety over normal fluctuations, especially if you’re not on insulin. There’s also a valid concern about misinterpretation without proper clinical context.
A good example is the widely spread belief—particularly on social media—that a completely flat glucose response is ideal. In reality, modest rises after eating are both normal and healthy; it’s excessive spikes or prolonged elevations that are problematic. Chasing an entirely flat line can lead to adopting unsustainable (and arguably dangerous) eating patterns that may cause more harm than good.
The counterpoints:
Used correctly, CGMs can do far more than track numbers; they can reveal the earliest signs of metabolic dysfunction, often years before standard labs would raise a flag. Furthermore, they give individuals a way to see how their unique physiology responds to real life:
- The foods they eat
- The workouts they do
- The sleep they get, and
- The stress they carry
That real-time feedback creates a powerful feedback loop — where small, strategic changes lead to measurable improvements you can see in days, not months. For many, that’s the difference between waiting until symptoms demand treatment and actively steering their health trajectory toward resilience and prevention.
Who Benefits Most
While CGMs were designed for people managing diabetes, their potential extends far beyond that group. In the right hands, they can be a powerful tool for anyone wanting to understand and improve their metabolic health, especially those in the following categories:
- People with signs of insulin resistance — Energy crashes, brain fog, weight changes, or poor workout recovery can all hint at glucose dysregulation. A CGM helps identify triggers and patterns.
- Individuals with elevated fasting glucose or A1c (prediabetes ranges or trending upward) — CGMs can reveal post‑meal spikes, dawn phenomenon, and timing effects so you can intervene earlier. If you have diabetes, CGMs can be valuable when used in partnership with your clinician; they’re standard of care for those on insulin.
- Those with a family history of metabolic or cardiovascular disease – If diabetes, heart disease, or metabolic syndrome runs in the family, early insights can be a proactive way to protect long-term health.
- Athletes and active individuals – Optimizing fueling, recovery, and performance requires knowing how your body responds to different training loads, nutrition strategies, and recovery protocols.
- Individuals managing inflammatory or autoimmune conditions – Blood sugar instability can exacerbate systemic inflammation and immune dysregulation. CGMs can help identify and stabilize patterns that may contribute to symptom flares.
- People with sleep or mood challenges – Glucose swings can impact sleep quality, stress resilience, mood regulation, and focus. Tracking these patterns can uncover links between blood sugar, rest, and emotional well-being.
Best Practices for using a CGM
Using a CGM for lifestyle and prevention is still in its early days. While the technology is promising, there are no universally accepted guidelines for non-diabetic use. That’s why working with a nutrition professional or clinician who understands metabolic health is so valuable — they can help you interpret patterns in context, avoid common missteps, and translate the numbers into practical strategies you can actually follow.
Remember, this isn’t about chasing a “perfect” glucose curve. It’s about using the data as one piece of your larger health picture—layered with other metrics, lab work, and your personal goals—to make changes that are sustainable and meaningful.
Practical Tips for using a CGM:
- Commit to at least 2–4 weeks. Wear the sensor long enough to capture your true baseline and see how different days, meals, and activities affect you. I suggest focusing on the first week for observation — avoid making big changes until you understand your natural patterns.
- Track beyond the numbers. Log food, sleep, mood, stress, workouts, and other symptoms in real time. These contextual notes are what make your CGM data actionable.
- Approach it with an experimental mindset. Think of your first CGM experience as a discovery phase—not a pass/fail test. Use it to explore how different choices affect your blood sugar, and resist the urge to “game” the data for perfection.
- Look for patterns, don’t obsess over specific points or readings. Our blood sugar is impacted by various factors and is a dynamic measurement. Single spikes or dips are normal; focus on recurring trends like large post-meal excursions, prolonged overnight elevations, or unusual variability.
- Integrate with other metrics. Pair CGM data with HRV, sleep tracking, lab work, and body composition analysis to connect the dots between glucose and overall metabolic health.
- Avoid overreacting. Remember: not all rises are “bad.” Normal glucose flexibility includes modest post-meal increases — especially with whole-food, nutrient-dense meals. The aim is stability and resilience, not a flatline.
Important Note: CGMs can be powerful tools for awareness and behavior change—but they aren’t for everyone. If you’re prone to anxiety over health data, or have a history of disordered eating, the constant feedback may be more stressful than helpful. In those cases, there are other effective ways to support blood sugar without round-the-clock tracking.
Bottom line
For many people, though, a short-term CGM trial—used in collaboration with a nutrition or health professional—can be eye-opening. It allows you to connect the dots between your daily choices and your metabolic responses, long before a standard lab might reveal a problem.
The value of a CGM isn’t in chasing a perfect number. Rather, the value of CGMs lies in using the insights to make sustainable, personalized changes that improve your energy, mood, and long-term health resilience.
Join my 4-Week CGM Program
If you’re ready to explore what your blood sugar is really doing—and learn how to use that information to your advantage—join my guided program:
Blood Sugar Mastery CGM Course →
⚠️ Disclaimer: This content is for educational purposes only and is not a substitute for personalized medical advice. Always consult a qualified healthcare provider before starting or changing any health-related program.
References
- Cleveland Clinic. Continuous Glucose Monitoring (CGM). Cleveland Clinic. Published June 20, 2023. Accessed September 13, 2025. https://my.clevelandclinic.org/health/articles/continuous-glucose-monitoring-cgm
- U.S. Food and Drug Administration. FDA clears first over-the-counter continuous glucose monitor. FDA. Published March 5, 2024. Accessed September 13, 2025. https://www.fda.gov/news-events/press-announcements/fda-clears-first-over-counter-continuous-glucose-monitor
- Berry SE, Valdes AM, Drew DA, et al. Human postprandial responses to food and potential for precision nutrition. Nat Med. 2020;26(6):964-973. doi:10.1038/s41591-020-0934-0
- Metwally AA, Perelman D, Park H, et al. Prediction of metabolic subphenotypes of type 2 diabetes via continuous glucose monitoring and machine learning. Nat Biomed Eng. 2025;9(8):1222-1239. doi:10.1038/s41551-024-01311-6
- Yang Y, Zhao LH, Li DD, et al. Association of sleep quality with glycemic variability assessed by flash glucose monitoring in patients with type 2 diabetes. Diabetol Metab Syndr. 2021;13(1):102. Published 2021 Sep 23. doi:10.1186/s13098-021-00720-w
Visceral Fat: The Hidden Risk Factor You Can Actually Target
Body composition tells us far more about metabolic health than weight or BMI ever could. Beyond the broad categories of fat mass and lean mass, one specific marker has an outsized impact on disease risk: visceral fat.
Unlike subcutaneous fat that sits under the skin, visceral fat accumulates deep in the abdominal cavity, wrapping around vital organs. It’s metabolically active in ways that can disrupt hormones, drive inflammation, and impair insulin sensitivity—even in people who appear lean.
Understanding visceral fat—and how it interacts with muscle mass—gives us a clearer, more actionable picture of health risk. It also shifts the focus from chasing an arbitrary weight to targeting specific, measurable changes that truly impact long-term health.
The Real Risk—Visceral Fat
Visceral fat is stored deep inside the abdominal cavity, surrounding organs like the liver, pancreas, and intestines. Unlike subcutaneous fat, which sits just under the skin, visceral fat is hidden and metabolically active — it influences hormone function, inflammation, and immune signaling in ways that can disrupt metabolic health.
It’s also the fat depot most strongly linked to chronic disease risk. Elevated visceral fat contributes to:
- Insulin resistance and impaired glucose tolerance
- Metabolic syndrome and type 2 diabetes
- Cardiovascular disease, hypertension, and cholesterol abnormalities
- Increased systemic inflammation
- Higher risk of cognitive decline and dementia
This is not just a concern for people in larger bodies. The so-called “skinny fat” phenomenon describes individuals with a normal BMI who still carry high levels of visceral fat, and face elevated metabolic risk. Conversely, some people classified as “overweight” may have relatively low visceral fat and higher muscle mass, which can be metabolically protective.
Muscle mass plays a critical role
Skeletal muscle is a major site for glucose uptake and storage, helping regulate blood sugar and improve insulin sensitivity. It also supports a higher resting metabolic rate, meaning more calories burned at rest, and releases myokines — signaling molecules that improve fat oxidation, glucose metabolism, and inflammation control.
In practical terms: more muscle generally means better metabolic flexibility and lower visceral fat risk.
Focusing on visceral fat and muscle mass together gives a much more accurate picture of metabolic health than weight or BMI alone—and creates clearer targets for meaningful intervention.
How to Track What Actually Matters
Measuring visceral fat and muscle mass used to require advanced imaging like CT or MRI scans — accurate, but costly and impractical for routine use. Now, accessible tools make it possible to estimate these markers in a clinic and now even at home!
Waist-to-Hip Ratio
One of the simplest ways to approximate visceral fat is by measuring your waist-to-hip ratio. A higher ratio indicates more abdominal fat, which often corresponds to higher visceral fat. Even without a tape measure, changes in how your clothes fit — especially around the waist — can be a practical indicator of progress.
Body Composition Scales
Consumer-grade devices like InBody, Tanita, or Etekcity can estimate visceral fat, muscle mass, and other metrics. Not all scales include visceral fat measurements, so it’s worth confirming before purchasing. While they’re not as precise as clinical imaging, they’re consistent enough for tracking trends over time.
Check out InBody H30 and get 15% off using this link
Professional Body Scans
Some healthcare offices and fitness facilities offer more advanced body composition assessments. These may include multi-frequency bioelectrical impedance, DEXA scans, or segmental muscle analysis, which provide more detailed insights into fat distribution and muscle balance.
Practical Tracking Tips:
- Pick your method and stick with it. Switching between devices or techniques makes it harder to compare results over time.
- Track at the same time of day. Morning, before eating or drinking, tends to give the most consistent results.
- Control for hydration. Dehydration or overhydration can skew bioelectrical impedance results, so best to be consistent with your hydration anyway — get my free guide here :)
- Pair objective data with subjective cues. Monitor how your clothes fit, your energy levels, and your exercise performance alongside scale or scan numbers.
- Look for trends, not single data points. Day-to-day fluctuations or even measurement errors are normal and happen. Don’t let it get to you; keep in mind that progress is measured over time.
- If you can’t get a scale that measures visceral fat, include waist circumference or waist-to-hip ratio. These remain simple, reliable indicators of metabolic risk.
It is worth repeating that there is no such thing as a perfect measurement, consistency and patterns over time are most helpful. Using the same tool, under similar conditions, at regular intervals builds a clearer picture of your progress towards improving muscle mass, lowering visceral fat, and ultimately better metabolic health.
What Actually Works for Reducing Visceral Fat
One of the unique things about visceral fat is that it’s the only type of fat that can be specifically reduced through targeted lifestyle changes. While ‘spot reduction’ isn’t possible for most fat depots, visceral fat is different, and in fact, responds more quickly to targeted interventions — independent of total weight loss.
1. Improve Diet Quality
- Prioritize protein and fiber to maintain lean muscle, regulate blood sugar, and support satiety.
- Eat the rainbow—colorful fruits and vegetables provide antioxidants that reduce inflammation and support metabolic health.
- Choose healthy fats from olive oil, nuts, seeds, avocados, and fatty fish; avoid trans fats altogether.
- Limit added sugars, refined carbs, and ultra-processed foods to reduce insulin resistance and central fat storage.
Looking for an easy place to start? Upgrade your breakfast → join the 7-Day Rainbow + Protein Challenge
7-Day Rainbow Protein Breakfast Challenge – fast win for glucose stability + consistency.
2. Train for Both Strength and Endurance
- Strength training builds muscle, which is protective against metabolic decline and helps reduce visceral fat over time.
- Aerobic exercise—150–300 minutes of moderate-intensity or 75–150 minutes of vigorous-intensity per week—lowers visceral fat even without total weight change. HIIT may provide additional benefits, especially for improved insulin sensitivity and weight loss, but the priority is consistent movement.
3. Sleep and Stress Matter
- Aim for 7–9 hours of quality sleep supports hormone regulation and reduce visceral fat risk.
- Chronic stress management—via mindfulness, yoga, breathwork, or other practices, helps lower cortisol, which can drive visceral fat accumulation.
4. Reduce Liquid Calories and Alcohol
- Limit alcohol intake, particularly binge patterns, which are strongly linked to visceral fat gain.
- Minimize or better still eliminate sugar-sweetened beverages, which promote abdominal fat through effects on insulin and appetite regulation.
5. Strategic Adjuncts
- Intermittent fasting can improve insulin sensitivity and fat oxidation for some individuals, but it’s not necessarily superior to consistent dietary improvements above.
- Pre- and probiotics may benefit visceral fat through gut microbiome improvements. However, it doesn’t seem to replace a foundational diet and lifestyle that is supportive of gut and microbiome health.
Sauna and cold exposure show promising early data but should complement—not replace—core habits. It is worth noting that cold plunges boost metabolic rate and may help with body fat reduction and improve insulin sensitivity — primarily via brown fat (known as brown adipose tissue [BAT]) activation.
The Bottom Line
Visceral fat is a powerful driver of metabolic risk that you can actively target and change. Focusing on diet quality, strength and endurance training, sleep, stress management, and smart adjuncts not only lowers visceral fat, but also builds the muscle and metabolic resilience that protect long-term health.
The goal isn’t to chase a lower scale weight. Instead, it’s to improve your body composition in ways that directly impact your risk for chronic disease, energy levels, and overall quality of life.
Ready to go deeper?
If you want to learn how to train your body to switch between fuel sources efficiently, regulate blood sugar, and protect metabolic health, join the Metabolic Flexibility Crash Course.
Explore the Metabolic Flexibility Crash Course →
References
- Lin S, Jensen MD. Human Adipose Tissue Metabolism in Obesity. J Obes Metab Syndr. 2025;34(2):105-119. doi:10.7570/jomes25025
- Sun Y, Lin X, Zou Z, et al. Association between visceral fat area and metabolic syndrome in individuals with normal body weight: insights from a Chinese health screening dataset. Lipids Health Dis. 2025;24(1):57. Published 2025 Feb 18. doi:10.1186/s12944-025-02482-0
- Richter EA, Bilan PJ, Klip A. A comprehensive view of muscle glucose uptake: regulation by insulin, contractile activity, and exercise. Physiol Rev. 2025;105(3):1867-1945. doi:10.1152/physrev.00033.2024
- Huang G, Pencina K, Li Z, et al. Effect of Protein Intake on Visceral Abdominal Fat and Metabolic Biomarkers in Older Men With Functional Limitations: Results From a Randomized Clinical Trial. J Gerontol A Biol Sci Med Sci. 2021;76(6):1084-1089. doi:10.1093/gerona/glab007
- Cavallo DN, Horino M, McCarthy WJ. Adult Intake of Minimally Processed Fruits and Vegetables: Associations with Cardiometabolic Disease Risk Factors. J Acad Nutr Diet. 2016;116(9):1387-1394. doi:10.1016/j.jand.2016.03.019
- Lehmann S, Retschlag U, Oberbach A, et al. Visceral fat mass dynamics in a 2-year randomized STrength versus ENdurance training trial in people with obesity. Diabetes Obes Metab. 2024;26(9):4087-4099. doi:10.1111/dom.15767
- Dutheil F, Lac G, Lesourd B, et al. Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE randomized trial. Int J Cardiol. 2013;168(4):3634-3642. doi:10.1016/j.ijcard.2013.05.012
- Kazibwe R, Chevli PA, Evans JK, et al. Association Between Alcohol Consumption and Ectopic Fat in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2023;12(18):e030470. doi:10.1161/JAHA.123.030470
- National Institutes of Health (NIH). Cool temperature alters human fat metabolism. NIH Research Matters. August 22, 2023. Accessed August 26, 2025. https://stagetestdomain3.nih.gov/news-events/nih-research-matters/cool-temperature-alters-human-fat-metabolism
Why the Scale is Lying to You: What Body Composition Tells Us About Metabolic Health
Most people have a complicated relationship with the scale. It's the most accessible data point, and one we’re taught to rely on from an early age at pediatrician check-ins.
But over time, and with the added pressure of fitting into beauty or athletic standards, it turns into something more emotionally charged. And that emotional weight tied to that number can be heavier than the physical one — and frankly, it's not even that useful.
Body weight doesn’t account for what your body is actually made of. It doesn’t reflect fat distribution or muscle density, for example. It can be swayed up and down by inflammation and fluid shifts. Most egregiously, it ignores the impact of fat storage and doesn’t allow for an important conversation about subcutaneous and deep fat deposits around your organs, where it can silently drive metabolic dysfunction.
Weight and BMI might be the default metrics, but they’re outdated. They tell us little about what matters most: how much muscle you have, how resilient your metabolism is, and whether your weight distribution is contributing to — or protecting you from — chronic disease.
That’s where body composition comes in. When we start looking at visceral fat and muscle mass instead of just “weight,” we get a far clearer picture of risk, resilience, and real progress.
Let’s break that down.
We’re Asking Too Much from the Scale
For all its flaws, the scale has some utility. It’s inexpensive, widely available, and for certain clinical scenarios, like monitoring for fluid retention in patients with heart failure or kidney disease, it provides a helpful data point. It's also useful in pediatric settings where linear growth and appropriate weight gain help monitor development.
But outside of those specific use cases, we tend to over-rely on it specifically for metabolic health.
Body weight alone doesn’t tell us what’s changing inside the body. That number includes everything—muscle, fat, bone, water, even food content in the gut. It fluctuates daily with hormonal shifts, hydration status, inflammation, and more, making it unreliable for tracking progress.
And even when weight changes reflect fat loss, the scale won’t tell you what kind of fat you’re losing—or gaining. It certainly won’t tell you if you’re building metabolically protective muscle mass.
Many people notice this firsthand: same weight on the scale, but clothes fit differently.
Relying solely on the scale can derail progress and distract from meaningful improvements in health markers, energy, and quality of life. It’s a blunt tool being asked to do a job above its pay grade.
Why BMI is Outdated
You might be wondering: if the scale is limited, what about BMI?
The Body Mass Index (BMI) is calculated using a simple formula: weight in kilograms divided by height in meters squared (referred to as “Quetelet Index”). It’s been widely used to screen for health risk based on categories ranging from underweight to overweight and obese.
But context matters.
BMI wasn’t developed for clinical practice. It was originally introduced in the 1830s by Belgian statistician Adolphe Quetelet to describe the “average man” for demographic studies, definitely not for diagnosing health or disease risk. Over a century later, physiologist Ancel Keys repurposed the formula in population health research. The choice was for its convenience, not its accuracy, and certainly not its applicability to individual clinical assessment.
Despite that, BMI was quickly adopted into medical guidelines and remains a dominant tool in routine care. But it has significant limitations.
First, it doesn’t distinguish between muscle and fat.
A lean, muscular person might be flagged as “overweight,” while someone with low muscle mass and high visceral fat might fall into a “normal” range. BMI also fails to account for age, sex, ethnicity, or fat distribution — factors that all have clinical relevance.
Second, the thresholds were based largely on studies of European male populations.
That makes it less predictive for people of different racial and ethnic backgrounds, body types, and ages. Risk patterns vary across groups, but BMI doesn’t reflect that nuance.
Third, there’s the issue of stigma.
BMI does not differentiate between lean muscle and fat. Athletes and those with high muscularity may be incorrectly classified as overweight or obese, while thin individuals with high visceral fat can be labeled healthy.
When BMI is used as the sole determinant of health, it can lead to biased care, delayed diagnoses, or inappropriate treatment plans. Clinically, it contributes to overgeneralizations and underassessment of actual metabolic markers.
Today, many experts agree: BMI may be a convenient screening tool at the population level, but it’s a poor substitute for a personalized, functional view of health. That includes assessing waist circumference, body composition, and most importantly, health behaviors and biomarkers that reflect metabolic function.
Summary Table: Key Criticisms of Body Mass Index (BMI)
| Flaw associated with BMI | Description |
| Population, not individual tool | Designed as a statistical average, not for clinical diagnosis |
| Ignores body composition | Cannot distinguish muscle mass, bone density, or fat distribution |
| Poor for non-European groups | Formula and cutoffs do not translate well across ethnicities, sex, or ages |
| Misses metabolic health | Does not account for fitness, genetics, or other metabolic risk factors |
| Stigma and clinical misuse | Can lead to inappropriate clinical decisions and patient harm |
| Inaccurate at extremes | Particularly inaccurate for very short/tall individuals, athletes, and elderly |
Body Composition 101: What the Scale Doesn’t Tell You
Body composition gives us a more precise view of what the body is made of—and which components actually influence health. Unlike weight or BMI, it accounts for distribution, density, and function. Here are the basics:
- Lean Mass: Muscle, bone, and water.
- Fat Mass: Includes subcutaneous fat (under the skin) and visceral fat (around organs).
- Muscle Mass: A major determinant of metabolic flexibility, insulin sensitivity, and glucose disposal.
- Visceral Fat: The more clinically relevant type of fat, strongly linked to cardiometabolic risk.
Practical Rankings for Metabolic Health & Home Use
| Marker | Why It Matters for Health | Can You Track It at Home? |
| Body Fat % | Helps differentiate between lean and fat mass. | Yes—most smart scales. |
| Visceral Fat Index | Strong predictor of insulin resistance, fatty liver, and cardiovascular risk. | Some consumer-grade scales include it, though reliability varies. |
| Muscle Mass | Correlates with improved metabolic function, blood sugar control, and reduced inflammation. | Yes—most InBody-type scales. |
| Lean Mass | Includes all non-fat tissue. Important for physical function and aging. | Common in home body comp devices. |
| Body Water % | Reflects hydration and inflammation, but is less useful on its own. | Standard on most digital scales. |
| Bone Mass | Useful for baseline health monitoring, but not dynamic in short-term tracking. | Included in many reports, though changes slowly. |
| Basal Metabolic Rate (BMR) | Reflects energy expenditure at rest—helpful for estimating needs, not a health marker itself. | Common on apps and smart scales. |
| BMI | Still shows up, but not useful alone for assessing health. | Default on most scales. |
Among these, visceral fat and muscle mass carry the most weight—no pun intended—when it comes to metabolic health.
In particular, muscle plays a central role in blood sugar regulation, hormone sensitivity, and inflammation resolution. It's not just a strength metric– it’s metabolically active tissue that directly supports glucose uptake and mitochondrial health. Increasing or maintaining muscle mass can improve metabolic markers independent of changes in body weight or BMI.
And unlike subcutaneous fat, visceral fat is hormonally active in ways that drive dysfunction. It’s associated with increased cortisol, inflammation, and impaired insulin sensitivity. That means two people with the same weight—or even the same BMI—can have drastically different risk profiles depending on how much visceral fat they carry.
In short: not all fat is equal, and not all weight loss is beneficial. Tracking body composition offers a more targeted, nuanced view of health progress—one that’s much harder to come by if you’re only looking at a number on the scale.
The Bottom Line
The scale is a simple and inexpensive tool, but it’s a poor proxy for health. If you’re seeking metabolic resilience, interested in preserving muscle, or reducing visceral fat, you need better data than weight or even BMI can provide.
If your goal is to reduce disease risk, improve energy, and support long-term health, body composition – especially muscle mass and visceral fat – are the better metrics to track. Let’s shift the conversation to function and metabolic protection — where it should be.
Ready to take the next step?
If you’re interested in learning more about the tools and rationale behind metabolic flexibility, you’ll love the free Metabolic Flexibility Crash Course. The course is packed with valuable insights on turning on the metabolic switch to optimize blood sugar, and protect long-term metabolic health, without obsessing over the scale.
Crash the Metabolic Health Crash Course
References
- National Heart, Lung, and Blood Institute. BMI tools. National Institutes of Health. Updated August 21, 2025. Accessed August 21, 2025. https://www.nhlbi.nih.gov/health/educational/lose_wt/bmitools.htm
- Gonzalez MC, Correia MITD, Heymsfield SB. A requiem for BMI in the clinical setting. Curr Opin Clin Nutr Metab Care. 2017;20(5):314-321. doi:10.1097/MCO.0000000000000395
- Wu Y, Li D, Vermund SH. Advantages and limitations of the body mass index (BMI) to assess adult obesity. Int J Environ Res Public Health. 2024;21(6):757. doi:10.3390/ijerph21060757
- Nadolsky K, Addison B, Agarwal M, et al. American Association of Clinical Endocrinology consensus statement: addressing stigma and bias in the diagnosis and management of patients with obesity/adiposity-based chronic disease and assessing bias and stigmatization as determinants of disease severity. Endocr Pract. 2023;29(6):417-427. doi:10.1016/j.eprac.2023.03.272
- Guerra Valencia J, Castillo-Paredes A, Gibaja-Arce C, Saavedra-Garcia L, Barengo NC. The association between lean-to-fat mass ratio and cardiometabolic abnormalities: an analytical cross-sectional study. J Clin Med Res. 2024;16(2-3):81-93. doi:10.14740/jocmr5096
- Khawaja T, Nied M, Wilgor A, Neeland IJ. Impact of visceral and hepatic fat on cardiometabolic health. Curr Cardiol Rep. 2024;26(11):1297-1307. doi:10.1007/s11886-024-02127-1
- Pagel-Langenickel I, Bao J, Pang L, Sack MN. The role of mitochondria in the pathophysiology of skeletal muscle insulin resistance. Endocr Rev. 2010;31(1):25-51. doi:10.1210/er.2009-0003
What Are Endocrine Disruptors?
How Everyday Chemicals Disrupt Hormones and What You Can Do About It
Endocrine-disrupting chemicals (EDCs) are environmental compounds that can interfere with the body’s hormone systems and alter how hormones are produced, transported, metabolized, or received at the cellular level. These disruptions may affect numerous systems in the body, including metabolism, reproduction, immune function, and neurological development.
Unlike acute toxins, EDCs often cause harm through low-dose and long-term exposure. This is especially significant during sensitive developmental windows such as in utero, early childhood, puberty, or pregnancy. These effects may not be immediately obvious but can contribute to chronic disease risk over time.
A key challenge with EDCs is that they do not follow the typical toxicology rule that “the dose makes the poison.” Small amounts – measured in parts per billion (ppb) or trillion (ppt) – have been shown to impact hormone-sensitive systems. This is partly because hormones themselves act at these extremely low concentrations in the body, making them vulnerable to even subtle external interference.
In addition, bioaccumulation – the build-up of chemicals in fat tissue, organs, or passed down across generations– compounds the problem. Many EDCs are lipophilic and persistent, meaning they remain in the body and the environment long after exposure. This is exemplified by the increasing detection of microplastics in human blood, tissues, and breastmilk—an indicator of how pervasive and long-lasting these exposures can be.
In this blog, we’ll explore:
- What EDCs are and where they’re most commonly found
- How they affect health according to current research
- Key strategies to reduce your exposure through environmental, dietary, and lifestyle interventions
What Exactly Are Endocrine Disruptors?
Endocrine-disrupting chemicals (EDCs) interfere with the body’s hormonal systems. They can mimic hormones, block hormone receptors, or alter how hormones are made, broken down, or used.
Because hormones regulate critical processes – like metabolism, growth, reproduction, and stress response – disrupting these pathways can have widespread effects.
These disruptions don’t require high doses. Many EDCs operate at very low concentrations, similar to how natural hormones function. That’s what makes them particularly difficult to regulate and detect, even though they may still cause meaningful biological changes.
Common Types of Endocrine Disruptors (EDCs)
EDCs come from a wide range of sources. Some of the most well-known include:
- BPA (Bisphenol A) – Found in can linings, plastic containers, and receipts.
- Phthalates – Used in soft plastics (like food packaging and shower curtains) and also hidden in “fragrance” in soaps, personal care products, and cleaning sprays.
- Parabens – Preservatives used in lotions, shampoos, and cosmetics.
- PFAS (Per- and polyfluoroalkyl substances) – Found in nonstick cookware, grease-resistant food wrappers, and some water-resistant fabrics.
- Dioxins – Industrial byproducts that accumulate in animal fats and dairy.
Organophosphate pesticides – Common in conventional produce, especially if not washed or peeled.
Where You’re Most Likely to Encounter EDCs
While some exposures come from industrial pollution or contaminated water, most people encounter EDCs through daily habits, especially via the kitchen and household environment:
- Plastics – Food packaging, storage containers, water bottles, and cling wrap.
- Fragrance – Found in soaps, shampoos, air fresheners, candles, laundry detergents, and cleaning sprays.
- Pesticides – Residues on non-organic fruits, vegetables, and grains.
- Nonstick coatings – Frying pans, rice cookers, air fryer baskets, baking sheets, and takeout containers.
- Tap water – May contain pesticide residues, pharmaceuticals, PFAS, and heavy metals depending on the local source.
- Dust and indoor air – Flame retardants, microplastics, and chemicals from building materials and furniture settle in household dust, especially in poorly ventilated spaces.
Even low-level exposures — when repeated daily over time — can accumulate and affect health, especially when the body’s detoxification pathways are already burdened.
Why Small Exposures Still Matter
Traditional toxicology focuses on identifying the dose of a chemical required to cause harm. While this holds true for many poisons, it doesn’t apply as neatly to endocrine-disrupting chemicals (EDCs). That’s because hormones themselves work at extremely low concentrations, and because they can bioaccumulate over time.
EDCs don’t just change hormone levels; they interfere with how hormones communicate. They can bind to receptors, altering feedback loops, or affecting how hormones are produced or broken down.
⚠️ Low Dose ≠ Low Risk
EDCs often follow non-monotonic dose-response curves (NMDR), meaning that small exposures can have different, and sometimes more potent, effects than larger ones. This makes standard toxicology testing, which focuses on high doses, insufficient to detect the true risks.
In other words: everyday exposure from water, air, packaging, and personal care products may be biologically active, even if it's not acutely toxic.
That’s partly because the endocrine system is designed to respond to small shifts in hormone levels. But that means that even very low-level exposures to hormone-mimicking chemicals can interfere with normal hormonal signaling functioning.
🧬 Bioaccumulation and Persistent Exposure
Many EDCs are lipophilic, meaning they’re fat-soluble and can accumulate in the body’s tissues over time. Like a bank account, once stored, they may remain for years, contributing to chronic, internal exposure even after the source is removed.
This is particularly relevant for persistent organic pollutants (POPs) like dioxins and certain pesticides, as well as microplastics, which are now being detected in human blood, placentas, and breast milk..
⏳ Timing > Dose
The timing of exposure is often more important than the dose. Hormone-sensitive periods, like prenatal development, childhood, puberty, and perimenopause are especially vulnerable to disruption. Effects may not show up immediately, but they can alter long-term disease risk – sometimes across generations.
Major Health Impacts of EDC Exposure
Endocrine-disrupting chemicals have been linked to a wide range of health effects. These aren’t hypothetical risks – they’ve been observed in human and animal studies, supported by mechanistic research, and reinforced by long-term population data.
The impacts vary depending on timing, duration, and individual susceptibility (including genetic, nutritional, and lifestyle factors). Exposure during sensitive periods, including prenatal development, can lead to greater disruption. Furthermore, they can be passed down during gestation and through breast milk.
Here are some of the most well-documented areas of concern:
🧠 Neurological and Cognitive Effects
EDCs can interfere with neurodevelopment, neuroendocrine regulation, and long-term cognitive function. Effects are especially significant with early-life or in utero exposure, but adult exposure during hormone-sensitive life stages may also contribute.
- Disruption of prenatal and childhood brain development (notably linked to BPA and phthalates)
- Associations with ADHD, learning and behavior challenges, and altered social behavior in children
- Impaired mood regulation, increased anxiety, and altered stress hormone response (via HPA axis dysregulation)
- Emerging evidence linking EDCs to neurodegeneration, including increased risk for Alzheimer’s disease and cognitive decline in later life, possibly via estrogen signaling pathways, inflammation, and mitochondrial stress
🧬 Metabolic and Cardiovascular Effects
Hormones regulate metabolism, appetite, insulin sensitivity, and cardiovascular function. EDCs that disrupt these systems can increase the risk for:
- Insulin resistance and type 2 diabetes, especially with phthalate and BPA exposure
- Thyroid hormone disruption, including elevated TSH and reduced free T3/T4 levels
- Cardiovascular disease (CVD) through lipid imbalance, endothelial dysfunction, and oxidative stress
- Chronic kidney disease (CKD), with studies showing associations between PFAS exposure and impaired kidney function and glomerular filtration rate
🧪 Immune Dysfunction and Inflammatory Disease
EDCs can dysregulate immune signaling, increase systemic inflammation, and alter the gut-immune axis. These disruptions have been linked to:
- Increased risk of allergic disease, including asthma and eczema
- Influence on autoimmune disease development, especially thyroid autoimmunity and systemic lupus
- Impact on autoinflammatory conditions, including mast cell activation and histamine intolerance
- Altered microbiome balance, intestinal permeability, and immune barrier function
♀️ Reproductive Health and Hormone-Related Cancers
Because many EDCs mimic or block estrogen, progesterone, and androgens, reproductive impacts are among the most clearly documented:
- Altered menstrual cycles, irregular ovulation, and earlier onset of puberty
- Menstrual irregularities, PCOS, endometriosis, fibroids
- Reduced fertility in both women and men (via ovarian dysfunction or impaired sperm quality), along with an increased risk of miscarriage
- Anti-androgenic effects in males (e.g., lower sperm quality, genital abnormalities)
- Earlier onset of puberty and delayed menopause as well as changes in estrogen and progesterone signaling
- Increased risk for hormone-related cancers—including breast, prostate, and endometrial cancers—linked to long-term estrogen receptor stimulation and impaired detoxification of carcinogenic intermediates
Even if each individual effect seems small, their combined and cumulative impact across multiple hormone-regulated systems makes EDCs a high priority for both public health and personal prevention strategies.
What You Can Do About EDCs
You don’t need to overhaul your entire life to lower your exposure to hormone-disrupting chemicals. Instead, a strategic approach can make a meaningful impact. A few targeted changes can make a measurable difference, especially when it comes to the exposures you encounter daily.
Here are three places to start:
Limit Exposure at the Source
The easiest wins come from upgrading the everyday items where EDCs are most likely to show up. Start with swaps that reduce plastic, fragrance, and chemical coatings, especially in high-impact areas (the more often you use it, the more of a priority it is to reduce it).
High-impact places to focus:
- Plastic food containers (switch to glass or stainless)
- Tap water (install a filter that removes PFAS, pesticides, and heavy metals)
- Fragrance-heavy products (ditch air fresheners, plug-ins, and scented cleaners)
- Nonstick cookware (replace with stainless, ceramic, or cast iron)
📝 Want step-by-step recommendations?
Download the Hormone-Smart Kitchen Guide here →
Support Your Detox Pathways
You don’t need some magic potion or tea to detox. You’re already detoxing every day, your body knows exactly what to do. But it does need consistent resources to keep up with modern exposures:
- Eat a fiber-rich diet to promote regular elimination
- Stay hydrated to support kidney and liver function
- Prioritize cruciferous vegetables (like broccoli, cauliflower, arugula) to aid hormone metabolism
- Get regular movement and sweat (through exercise or sauna) to assist excretion
- Support gut health to enhance the microbiome’s role in detox and immune regulation
- Minimize alcohol and ultra-processed foods, which burden liver detox pathways
Reduce Household Chemical Load
Your home is where you spend the most time — and often where the greatest exposures add up. Focus on these practical steps:
- Choose unscented, EWG-verified personal care and cleaning products
- Vacuum and dust regularly to reduce EDC-containing particles
- Open windows daily to increase ventilation
- Filter indoor air using HEPA filters or plants known for air purification
- Wash hands before eating and after handling receipts, plastic, or cleaning products
In Conclusion
We may not be able to avoid endocrine disruptors entirely, but we can absolutely reduce our everyday exposure — and support our bodies in the process. The key is to start with small, intentional changes that add up over time.
You don’t need to be perfect — you just need to be aware. Every step you take to limit exposure and support detox is a powerful investment in your hormonal health and long-term vitality.
References
- Ahn C, Jeung EB. Endocrine-Disrupting Chemicals and Disease Endpoints. Int J Mol Sci. 2023;24(6):5342. Published 2023 Mar 10. doi:10.3390/ijms24065342
- Vandenberg LN, Colborn T, Hayes TB, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378-455. doi:10.1210/er.2011-1050
- Roslan NS, Lee YY, Ibrahim YS, et al. Detection of microplastics in human tissues and organs: A scoping review. J Glob Health. 2024;14:04179. Published 2024 Aug 23. doi:10.7189/jogh.14.04179
- United States EPA, 2023. Overview of Endocrine Disruption. Link
- National Institute of Environmental Health Sciences. Endocrine Disruptors. NIEHS. Updated April 1, 2024. Accessed May 15, 2025. https://www.niehs.nih.gov/health/topics/agents/endocrine
- Vandenberg LN, Colborn T, Hayes TB, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378-455. doi:10.1210/er.2011-1050
- Hill CE, Myers JP, Vandenberg LN. Nonmonotonic Dose-Response Curves Occur in Dose Ranges That Are Relevant to Regulatory Decision-Making. Dose Response. 2018;16(3):1559325818798282. Published 2018 Sep 13. doi:10.1177/1559325818798282
- Green, M., Harvey, A., Finger, B., & Tarulli, G. Endocrine disrupting chemicals: impacts on human fertility and fecundity during the peri-conception period.. Environmental research. 2020 https://doi.org/10.1016/j.envres.2020.110694.
- Gore AC, Chappell VA, Fenton SE, et al. EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocr Rev. 2015;36(6):E1-E150. doi:10.1210/er.2015-1010
- Yang Z, Zhang J, Wang M, et al. Prenatal endocrine-disrupting chemicals exposure and impact on offspring neurodevelopment: A systematic review and meta-analysis. Neurotoxicology. 2024;103:335-357. doi:10.1016/j.neuro.2024.07.006
- Su FC, Wei YC, Sun CY, et al. Endocrine-Disrupting Chemicals Exposure and Neurocognitive Function in the General Population: A Community-Based Study. Toxics. 2024;12(7):514. Published 2024 Jul 17. doi:10.3390/toxics12070514
- Dagar M, Kumari P, Mirza AMW, et al. The Hidden Threat: Endocrine Disruptors and Their Impact on Insulin Resistance. Cureus. 2023;15(10):e47282. Published 2023 Oct 18. doi:10.7759/cureus.47282
- Zhang X, Flaws JA, Spinella MJ, Irudayaraj J. The Relationship between Typical Environmental Endocrine Disruptors and Kidney Disease. Toxics. 2022;11(1):32. Published 2022 Dec 29. doi:10.3390/toxics11010032
- Liu Z, Lu Y, Zhong K, Wang C, Xu X. The associations between endocrine disrupting chemicals and markers of inflammation and immune responses: A systematic review and meta-analysis. Ecotoxicol Environ Saf. 2022;234:113382. doi:10.1016/j.ecoenv.2022.113382
- Calero-Medina L, Jimenez-Casquet MJ, Heras-Gonzalez L, et al. Dietary exposure to endocrine disruptors in gut microbiota: A systematic review. Sci Total Environ. 2023;886:163991. doi:10.1016/j.scitotenv.2023.163991
- Laws MJ, Neff AM, Brehm E, Warner GR, Flaws JA. Endocrine disrupting chemicals and reproductive disorders in women, men, and animal models. Adv Pharmacol. 2021;92:151-190. doi:10.1016/bs.apha.2021.03.008
Are Your Hormones Making You Histamine Intolerant?
The Missing Piece in Histamine Intolerance
If you’ve struggled with bloating, headaches, anxiety, insomnia, or worsening PMS, you may have focused on food as the primary trigger—eliminating high-histamine foods, taking antihistamines, or trying supplements—only to find that your symptoms still fluctuate.
"What if the real issue isn’t just what you eat but how your hormones interact with histamine?
The connection between histamine and estrogen is often overlooked, but it could explain why your symptoms:
- Get worse before your period
- Flare up around ovulation
- Intensify during perimenopause
- Begin or worsen after starting birth control or hormone replacement therapy (HRT)
Understanding how estrogen and histamine fuel each other can help you take control of your symptoms.
The Estrogen-Histamine Cycle
Histamine isn’t just involved in allergies—it plays a key role in digestion, immune function, and nervous system regulation. But when histamine builds up in the body, it can trigger symptoms like headaches, bloating, nausea, and inflammation.
Estrogen and histamine interact in ways that may worsen histamine intolerance.
- Estrogen stimulates mast cells to release histamine. When estrogen levels rise, histamine production increases.
- Histamine triggers more estrogen production. Once released, histamine signals the ovaries to produce more estrogen, creating a cycle that amplifies symptoms.
- Estrogen reduces DAO (diamine oxidase) enzyme activity. DAO is responsible for breaking down histamine in the gut. When estrogen suppresses DAO, histamine clearance slows, leading to a buildup.
This explains why histamine-related symptoms tend to spike during:
- Ovulation, when estrogen is at its highest
- The luteal phase (before your period), when estrogen levels drop after peaking
- Perimenopause, when estrogen levels fluctuate unpredictably
- When using birth control or HRT, which can introduce additional estrogen into the system
The Role of Birth Control and HRT
Many women report that their histamine-related symptoms began or worsened after starting hormonal birth control or HRT. While research is still emerging, some evidence suggests that exogenous estrogen (from birth control or HRT) may contribute to histamine intolerance.
- Estrogen has been shown to increase histamine activity, suggesting that hormonal therapies may worsen histamine-related symptoms in some individuals.
- Both estrogen and progesterone can reduce DAO activity, which is essential for breaking down histamine. When DAO is suppressed, histamine accumulates, leading to symptoms such as bloating, headaches, and skin reactions.
However, the research is not entirely conclusive:
- Most studies on HRT and birth control focus on cardiovascular, cancer, and bone health risks, rather than histamine-related symptoms.
- There is no definitive clinical research proving that HRT or birth control directly causes histamine intolerance—only strong correlations.
Women experiencing worsening histamine symptoms after starting hormonal therapy may benefit from monitoring symptoms and exploring alternative hormone-balancing strategies.
How to Break the Estrogen-Histamine Cycle
If you suspect that estrogen is making your histamine intolerance worse, there are ways to restore balance.
Support Estrogen Metabolism
The liver and gut play a major role in breaking down and eliminating excess estrogen. If either system is sluggish, estrogen can recirculate in the body, triggering histamine release.
- Eat cruciferous vegetables like broccoli, Brussels sprouts, and cabbage to support estrogen detoxification.
- Increase fiber intake from flaxseeds and chia seeds to help eliminate excess estrogen through the gut.
- Support liver function with DIM (diindolylmethane), calcium d-glucarate, and milk thistle.

Improve DAO Enzyme Function
Since estrogen can suppress DAO activity, increasing DAO production can help manage histamine symptoms.
- Boost DAO production with vitamin B6, magnesium, and copper, found in foods like poultry, salmon, and pumpkin seeds.
- Reduce DAO-blocking foods such as alcohol and black or green tea, which can slow histamine breakdown.
Stabilize Mast Cells to Reduce Histamine Release
Since mast cells release histamine in response to estrogen, reducing mast cell activation can help prevent excessive histamine buildup.
- Quercetin, found in apples, onions, and capers, helps stabilize mast cells.
- Vitamin C supports mast cell balance and acts as a natural antihistamine.
- Stinging nettle reduces histamine release and inflammation.
The Bottom Line
If you have been focusing only on food triggers without considering hormonal fluctuations, you may be missing a critical piece of the puzzle.
Histamine intolerance is not just about diet; it is about how your body processes histamine and estrogen together.
By supporting estrogen metabolism, enhancing DAO function, and stabilizing mast cells, you can better manage histamine symptoms and improve overall resilience.
For a comprehensive, step-by-step guide to managing histamine intolerance naturally, download the Estrogen + Histamine Guide here.
References
- Bonds RS, Midoro-Horiuti T. Estrogen effects in allergy and asthma. Curr Opin Allergy Clin Immunol. 2013;13(1):92-99. doi:10.1097/ACI.0b013e32835a6dd6
- Guo X, Xu X, Li T, et al. NLRP3 inflammasome activation of mast cells by estrogen via the nuclear-initiated signaling pathway contributes to the development of endometriosis. Front Immunol. 2021;12:749979. https://doi.org/10.3389/fimmu.2021.749979
- Zimna AI, Wróblewski H, Dubaj M, et al. Histamine intolerance caused by Diamine Oxidase (DAO) deficiency – case report. J Pre-Clin Clin Res. 2022;16(3):81-84. https://doi.org/10.26444/jpccr/153097
- Pham L, Baiocchi L, Kennedy L, et al. The interplay between mast cells, pineal gland, and circadian rhythm: Links between histamine, melatonin, and inflammatory mediators. J Pineal Res. 2021;70(2):e12699. https://doi.org/10.1111/jpi.12699
- Pal S, Gasheva OY, Zawieja DC, et al. Histamine-mediated autocrine signaling in mesenteric perilymphatic mast cells. Am J Physiol Regul Integr Comp Physiol. 2020;318(3):R590-R604. https://doi.org/10.1152/ajpregu.00255.2019
- Honda T, Nishio Y, Sakai H, et al. Calcium/calmodulin-dependent regulation of Rac GTPases and Akt in histamine-induced chemotaxis of mast cells. Cell Signal. 2021;83:109973. https://doi.org/10.1016/j.cellsig.2021.109973
Natural Solutions for Histamine Intolerance: A Root-Cause Approach
If you’ve been struggling with histamine-related symptoms—bloating, headaches, anxiety, PMS, or skin flare-ups—you’ve probably tried everything from food eliminations to antihistamines like Pepcid or Zyrtec.
These strategies might help in the short term, but they don’t fix the deeper issue: the root cause of why your body is struggling to break down histamine in the first place.
A true root-cause approach looks beyond symptom management and focuses on supporting histamine metabolism, gut health, and hormone balance so your body can regulate histamine naturally.
How to Naturally Support Histamine Clearance
Your body has built-in systems to break down histamine efficiently—but only when those systems are working properly. The key to long-term relief is supporting:
- Enzymes that break down histamine (like DAO and HNMT)
- The gut microbiome (to prevent histamine buildup and estrogen recirculation)
- Liver detox pathways (to clear histamine and estrogen effectively)
- Nutrients that regulate histamine production and inflammation
Here’s where to start:
1. Nutrients That Support Histamine Breakdown
Your body relies on specific enzymes—diamine oxidase (DAO) and histamine-N-methyltransferase (HNMT)—to break down histamine. If these enzymes aren’t working efficiently, histamine builds up, leading to symptoms.
These nutrients help:
- Vitamin C – A natural antihistamine that stabilizes mast cells and reduces histamine release. Found in bell peppers, citrus fruits, and kiwi.
- Vitamin B6 – Supports DAO enzyme production, which helps clear histamine from the body. Found in bananas, poultry, and sunflower seeds.
- Magnesium – Helps regulate histamine metabolism and prevent overproduction. Found in leafy greens, nuts, and seeds.
2. Herbs and Polyphenols That Stabilize Mast Cells
Mast cells release histamine as part of an immune response, but in histamine intolerance, they can become overactive. Certain plant compounds can help stabilize mast cells and reduce excessive histamine release.
- Quercetin – A potent flavonoid that helps stabilize mast cells and reduce inflammation. Found in apples, onions, and capers.
- Stinging Nettle – Traditionally used for allergies, nettle inhibits histamine release and supports immune balance.
- Curcumin – Found in turmeric, curcumin has anti-inflammatory and mast-cell stabilizing properties.
3. Gut-Supportive Compounds
Since the gut microbiome plays a major role in histamine metabolism, supporting gut health is essential for reducing histamine intolerance.
- Probiotics (Carefully Chosen) – Not all probiotics are beneficial for histamine intolerance. Look for strains like Bifidobacterium infantis and Lactobacillus plantarum, which help regulate histamine without increasing its production.
- Prebiotic Fibers –Foods like artichokes, asparagus, and green bananas feed beneficial gut bacteria and support DAO production.
- Glutamine – Helps heal the gut lining and reduce inflammation that can trigger histamine release.
4. Liver Detox Support
Your liver is responsible for clearing both histamine and excess estrogen. If detox pathways are sluggish, histamine can build up in the body.
- Sulfur-Rich Vegetables – Cruciferous veggies like broccoli, cabbage, and Brussels sprouts support estrogen and histamine metabolism.
- Milk Thistle – Supports liver detox and helps eliminate excess histamine and estrogen.
- Dandelion Root – A gentle liver tonic that promotes bile flow and estrogen clearance.
A Holistic Approach for Long-Term Relief
Managing histamine intolerance isn’t about avoiding high-histamine foods forever or relying on antihistamines. It’s about giving your body the tools it needs to regulate histamine naturally.
The right nutrients, gut support, and hormone balance strategies can help reduce histamine symptoms while addressing the root causes—so you can finally feel better.
Want a step-by-step plan?
📥 Download the full Estrogen + Histamine Guide here →
Inside, you’ll find a comprehensive approach to histamine intolerance, including food strategies, supplements, and practical tools to support your body naturally.
References:
- Fiorani M, Del Vecchio LE, Dargenio P, et al. Histamine-producing bacteria and their role in gastrointestinal disorders. Expert Rev Gastroenterol Hepatol. 2023;17(7):709-718. doi:10.1080/17474124.2023.2230865.
https://doi.org/10.1080/17474124.2023.2230865 - Khan M, Khan ZA, Naeem A, et al. Effect of dietary modification for targeting histamine activity in patients of allergic rhinitis: a randomized open-label study. Research Square. Published 2020. doi:10.21203/rs.3.rs-25717/v1.
https://doi.org/10.21203/rs.3.rs-25717/v1 - Cao M, Gao Y. Mast cell stabilizers: from pathogenic roles to targeting therapies. Front Immunol. 2024;15:1418897. Published August 1, 2024. doi:10.3389/fimmu.2024.1418897.
https://doi.org/10.3389/fimmu.2024.1418897 - Zeng J, Hao J, Yang Z, et al. Anti-allergic effect of dietary polyphenols curcumin and epigallocatechin gallate via anti-degranulation in IgE/antigen-stimulated mast cell model: A lipidomics perspective. Metabolites. 2023;13(5):628. Published May 5, 2023. doi:10.3390/metabo13050628.
https://doi.org/10.3390/metabo13050628 - Cheng W, Lu J, Li B, et al. Effect of functional oligosaccharides and ordinary dietary fiber on intestinal microbiota diversity. Front Microbiol. 2017;8:1750. Published September 20, 2017. doi:10.3389/fmicb.2017.01750.
https://doi.org/10.3389/fmicb.2017.01750 - Basnet J, Eissa MA, Cardozo LLY, Romero DG, Rezq S. Impact of probiotics and prebiotics on gut microbiome and hormonal regulation. Gastrointest Disord. 2024;6(4):801-815. doi:10.3390/gidisord6040056.
https://doi.org/10.3390/gidisord6040056
Can Your Gut Make You Histamine Intolerant? The Microbiome-Histamine Connection
If you have been dealing with histamine intolerance, you have likely been told to focus on avoiding high-histamine foods. While diet plays a role, histamine overload is not just about what you eat—it is about how your body processes and eliminates histamine.
Why Gut Health Is the Missing Piece in Histamine Intolerance
Your gut microbiome is one of the most important regulators of histamine metabolism. If your digestion is sluggish, your gut bacteria is out of balance, or your intestinal barrier is compromised, histamine intolerance can become significantly worse.
If you experience histamine-related symptoms such as bloating, nausea, acid reflux, skin rashes, or headaches, your gut may be driving the problem.
Let’s break down how the microbiome impacts histamine levels—and what you can do to fix it.
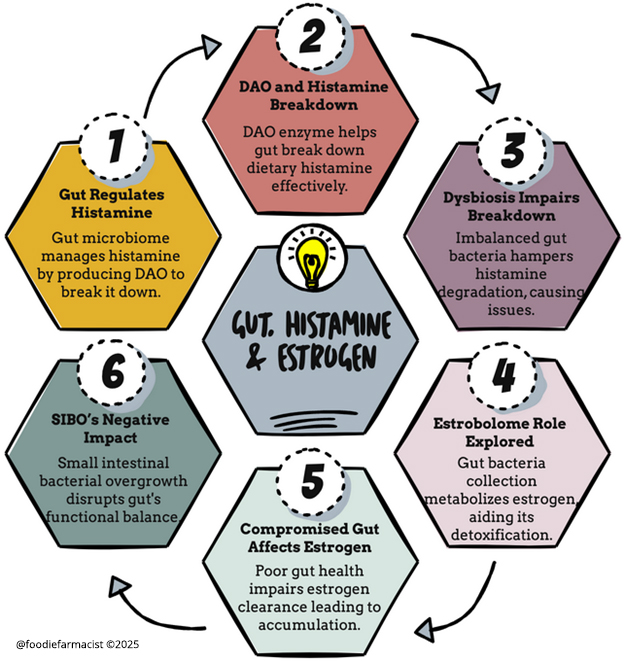
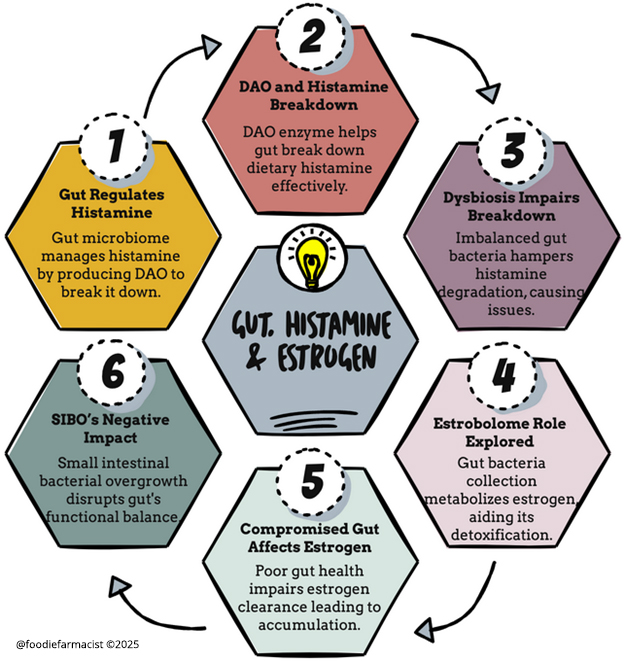
How the Gut Regulates Histamine
Histamine is produced and broken down in multiple areas of the body, but the gut is one of the primary control centers. There are three main ways your gut impacts histamine levels:
1. Certain Gut Bacteria Produce Histamine
Some gut bacteria naturally produce histamine as part of their metabolism. If these histamine-producing bacteria overgrow, histamine levels in the body can rise, leading to symptoms such as bloating, headaches, and flushing.
- Histamine-producing bacteria include:
- Morganella morganii
- Klebsiella pneumoniae
- Escherichia coli (certain strains)
If your microbiome is imbalanced—whether due to dysbiosis, SIBO (small intestinal bacterial overgrowth), or low gut diversity—you may have more histamine-producing bacteria than histamine-degrading ones. Stool testing through companies like DSL GI Map can help identify these imbalances.
2. The Gut Produces DAO (The Histamine-Breaking Enzyme)
DAO (diamine oxidase) is the main enzyme responsible for breaking down histamine from food. It is produced in the gut lining, which means that if gut health is compromised, DAO production may decline.
Factors that can reduce DAO production include:
- Leaky gut (intestinal permeability)
- Chronic inflammation or gut infections
- Food sensitivities that trigger gut irritation
- Certain medications (such as NSAIDs and proton pump inhibitors)
If DAO levels are too low, even a small amount of histamine from food can trigger symptoms.
3. The Gut Helps Eliminate Excess Histamine and Estrogen
Your gut microbiome also plays a crucial role in estrogen metabolism. The estrobolome (a subset of gut bacteria) helps break down and eliminate estrogen. If this process is disrupted, estrogen can recirculate in the body, further increasing histamine levels.
This means that if you have histamine intolerance and your digestion is slow or your microbiome is out of balance, you may also be holding onto excess estrogen—which can further fuel the histamine cycle.
Why Some Probiotics Can Make Histamine Intolerance Worse
Probiotics are often recommended for gut health, but not all probiotics are beneficial for histamine intolerance. Some strains actually produce histamine, which can worsen symptoms.
- Probiotics that may increase histamine:
- Lactobacillus casei
- Lactobacillus bulgaricus
- Lactobacillus reuteri
If you have histamine intolerance, taking the wrong probiotic could actually make symptoms worse, especially if your microbiome is already imbalanced.
The Right Gut-Health Strategies for Histamine Intolerance
Instead of focusing solely on food eliminations, addressing gut health can help regulate histamine metabolism and improve tolerance over time.
1. Support the Gut Lining and DAO Production
- Increase nutrients that support DAO enzyme production, such as vitamin B6, magnesium, and zinc.
- Reduce gut inflammation by avoiding processed foods, alcohol, and excessive caffeine.
- Incorporate gut-healing foods such as bone broth, aloe vera, and glutamine.
2. Focus on Probiotics That Degrade Histamine
Instead of taking general probiotics, focus on strains that help break down histamine rather than produce it.
- Histamine-degrading probiotics include:
- Bifidobacterium infantis
- Bifidobacterium longum
- Lactobacillus plantarum
These strains can help restore microbial balance and improve histamine tolerance over time.
3. Improve Gut Motility and Digestion
- Increase fiber intake from vegetables and flaxseeds to help clear histamine and estrogen.
- Support digestive enzymes and bile flow with bitters, ginger, and dandelion root.
- Hydrate properly to ensure smooth digestion and detoxification.
The Bottom Line
If you are struggling with histamine intolerance, focusing only on food eliminations will not solve the problem. Your gut plays a critical role in how your body processes and eliminates histamine, and if your microbiome is imbalanced, histamine intolerance will persist.
By improving gut health, increasing DAO activity, and choosing the right probiotics, you can build long-term resilience against histamine-related symptoms.
For a full step-by-step plan on managing histamine intolerance through gut health, download the Estrogen + Histamine Guide here.
References:
- Fiorani M, Del Vecchio LE, Dargenio P, et al. Histamine-producing bacteria and their role in gastrointestinal disorders. Expert Rev Gastroenterol Hepatol. 2023;17(7):709-718. doi:10.1080/17474124.2023.2230865
- Engevik K, Edens R, Engevik AC, Engevik MA, Horvath T. Production of histamine by diverse gut bacteria can activate intestinal HRH1 and promote calcium mobilization. Physiology. 2024;39(s1):2142. doi:10.1152/physiol.2024.39.s1.2142
- Mou Z, Yang Y, Hall AB, Jiang X. The taxonomic distribution of histamine-secreting bacteria in the human gut microbiome. BMC Genomics. 2021;22(1):Article 4. doi:10.1186/s12864-021-08004-3
- Smolinska S, Winiarska E, Głobińska A, Jutel M. Histamine: A mediator of intestinal disorders—a review. Metabolites. 2022;12(10):895. doi:10.3390/metabo12100895
- Sánchez-Pérez S, Comas-Basté O, Duelo A, et al. Intestinal dysbiosis in patients with histamine intolerance. Nutrients. 2022;14(9):1774. doi:10.3390/nu14091774
- Kumari N, Kumari R, Dua A, et al. From gut to hormones: Unraveling the role of gut microbiota in (phyto)estrogen modulation in health and disease. Mol Nutr Food Res. 2024;68(6):e2300688. doi:10.1002/mnfr.202300688
- Hu S, Ding Q, Zhang W, Kang M, Ma J, Zhao L. Gut microbial beta-glucuronidase: a vital regulator in female estrogen metabolism. Gut Microbes. 2023;15(1):2236749. doi:10.1080/19490976.2023.2236749
- Barber TM, Kabisch S, Pfeiffer AFH, Weickert MO. The health benefits of dietary fibre. Nutrients. 2020;12(10):3209. Published 2020 Oct 21. doi:10.3390/nu12103209
Histamine, Estrogen, and the Gut: The Overlooked Connection
You’ve tried everything for your PMS, perimenopause symptoms, or unexplained digestive issues—yet nothing seems to work. Maybe you’ve been told it’s just your hormones, or perhaps you’ve been given standard advice for acid reflux, allergies, or anxiety without much relief.
What if these symptoms were all connected?
Histamine, commonly known for its role in allergic reactions, also influences hormonal balance, digestion, and nervous system function. If you’re struggling with persistent symptoms, histamine intolerance might be the missing link.
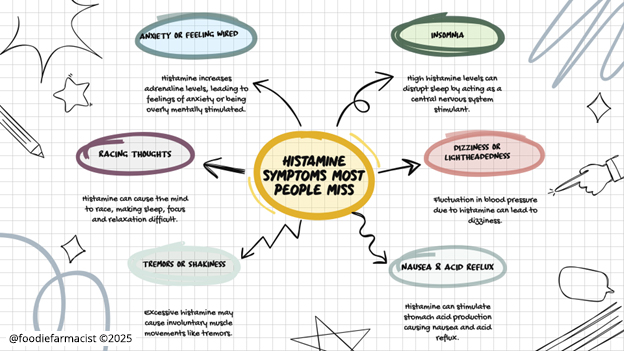
The Histamine Symptoms Most People Miss
Most people associate histamine with allergies—runny noses, sneezing, and itchy eyes. But histamine intolerance can also manifest in unexpected ways, including:
- Anxiety or feeling wired – Histamine increases adrenaline, making you feel restless, overstimulated, or jittery.
- Insomnia – High histamine levels can act as a central nervous system stimulant, making it harder to fall or stay asleep.
- Racing thoughts – Histamine can speed up brain activity, leading to difficulty focusing or relaxing.
- Dizziness or lightheadedness – Histamine-related blood pressure fluctuations can cause dizziness.
- Tremors or shakiness – Excess histamine may trigger involuntary muscle movements like tremors or twitching.
- Nausea & acid reflux – Histamine stimulates stomach acid production, which can contribute to nausea, heartburn, and digestive discomfort.
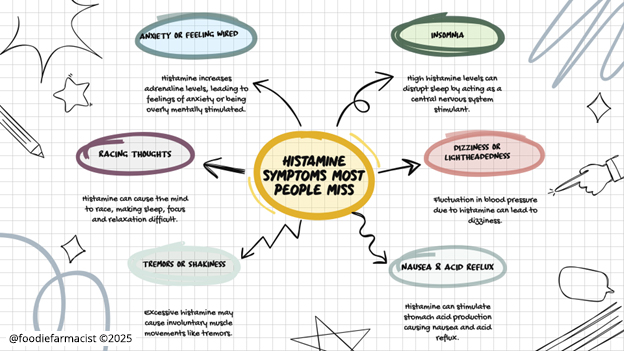
Many of these symptoms overlap with hormonal imbalances, perimenopause, or even anxiety disorders—which is why histamine intolerance is so often overlooked.
Why Is Pepcid All Over Social Media?
Recently, Pepcid (famotidine) has gained traction online as a quick fix for histamine intolerance. It’s an H2 receptor blocker, meaning it reduces histamine’s effects in the stomach, particularly by lowering acid production.
For some, this provides symptom relief—especially for reflux, nausea, and even certain systemic histamine reactions.
But here’s the thing: Pepcid only addresses part of the problem.
What You Should Know Before Using Pepcid for Histamine Issues
Like many medications, Pepcid treats symptoms, not root causes. While it can help in the short term, long-term use raises some concerns:
- It can deplete essential nutrients. H2 blockers like Pepcid can reduce absorption of vitamin B12, magnesium, and iron—nutrients already crucial for hormone balance and gut health. Learn more about drug-nutrient depletions here.
- It doesn’t address the real drivers of histamine intolerance. If estrogen dominance or gut dysbiosis are fueling your histamine issues, suppressing symptoms won’t solve the underlying problem.
- It may disrupt digestion over time. Stomach acid plays an essential role in breaking down food and absorbing nutrients. Long-term suppression can contribute to further imbalances.
Finding a simple, affordable solution like Pepcid can be helpful in a pinch, but a holistic approach that supports histamine metabolism, hormone balance, and gut health is key for long-term relief.
Histamine, Estrogen, and the Gut: A Vicious Cycle
Histamine and estrogen are closely linked—meaning that hormonal fluctuations can drive histamine symptoms, and vice versa.
- Estrogen triggers histamine release from mast cells, increasing symptoms like headaches, bloating, and anxiety.
- Histamine stimulates more estrogen production, creating a feedback loop that can make PMS and perimenopause symptoms worse.
- Estrogen blocks DAO (diamine oxidase), the enzyme that breaks down histamine, leading to buildup in the body.
This explains why histamine-related symptoms tend to peak before your period, during ovulation, or throughout perimenopause.
And because the gut plays a key role in clearing both estrogen and histamine, poor gut health can make everything worse.
The Root-Cause Approach: What You Can Do
Instead of relying on medications alone, addressing the underlying causes of histamine intolerance will help your body handle histamine more effectively.
- Support estrogen metabolism – Increase fiber (flax, cruciferous vegetables) and liver-supporting nutrients like DIM and milk thistle to help clear excess estrogen.
- Improve gut health – Focus on microbiome-friendly foods, prebiotic fibers, and gut-lining support like glutamine to improve histamine breakdown.
- Boost histamine metabolism naturally – Support DAO enzyme production with vitamin C, B6, magnesium, and quercetin.
This isn’t about quick fixes—it’s about building resilience so your body can process histamine effectively.
Want to take a deeper dive into how hormones, histamine, and gut health intersect?
Join the Estrogen + Histamine Guide WAITLIST here
It’s time to get to the root cause—so you can stop managing symptoms and start feeling like yourself again.
Simple Constipation Fixes for Better Digestion, Hormones, and Energy
Poop isn’t exactly dinner-table conversation. But your bathroom habits—how often you go, how easily it happens, and even how it looks—can reveal a lot about your health.
Take constipation, for example. Many assume it’s just part of life, something to tolerate or ignore. But what if your daily (or not-so-daily) trips to the bathroom are silently shaping other aspects of your well-being? Your energy levels, PMS symptoms, and even your mood could all be linked to how well your digestion is functioning.
Let’s dive into a real-world example that shows how working on the basics of digestion can unlock a ripple effect of improvements you didn’t even know were connected.
Meet Amy: A Case Study in Hormonal Balance and Gut Health
Amy, a 38-year-old self-employed designer, came to me feeling utterly drained. Her biggest complaints? Debilitating PMS symptoms, year-round allergies, and the kind of fatigue and brain fog that made it tough to stay focused on her work.
During our first session, Amy also mentioned she’d always had digestive issues—bloating after meals, occasional heartburn, and irregular bowel movements every 2–3 days that were often difficult to pass. “But that’s just how it’s always been,” she shrugged.
Amy didn’t realize how much her digestion might be impacting her hormones and energy levels. But as we reviewed her health history and symptoms in more detail, it became clear that her gut health was playing a much bigger role than she thought.
The Plan: Laying the Groundwork for Better Gut Health
Amy came to me frustrated and overwhelmed, feeling like her body was working against her. She knew something wasn’t right but couldn’t put her finger on the root cause – she felt like she was playing whack a mole with her symptoms.
Her heavy PMS symptoms, allergies, and relentless fatigue seemed like separate issues. Just when she thought she figured out a trigger, something would change!
It wasn’t until we started peeling back the layers of her health history that a hidden pattern emerged—her gut health was a key piece of the puzzle.
Instead of jumping to advanced testing, we began with some basics that aren’t usually fun enough to be a Tiktok trend. These are foundational strategies that don’t just support digestion but also set the stage for hormonal and overall health. Here’s what we uncovered and the steps we took:
1. Experimenting with Safer Fiber Options
When Amy tried increasing fiber in the past, it made her bloating and discomfort worse, which didn’t make any sense and left her discouraged.
Together, we explored a different approach: low-FODMAP fibers. By focusing on gentler options—like cooked zucchini, carrots, spinach, and firm bananas—we found foods that nourished her microbiome without triggering her symptoms.
This small tweak made a big difference. As her bloating eased, Amy realized that finding the right balance of fiber wasn’t about eating more but eating smarter. This gave us a big clue about what was going on “under the hood” even though we didn’t test for it.
2. Prioritizing Hydration with Electrolytes
Water alone wasn’t cutting it for Amy. Her busy mornings were usually coffee fueled and her long days meant she often forgot to hydrate until late afternoon, which only compounded her sluggish digestion.
So we emphasized starting the day with water. And we added a pinch of sea salt and a squeeze of lemon to her water in the morning, a simple electrolyte hack to help her body retain fluids and support optimal motility.
There’s “drink more water” and then there’s hydration <insert jazz hands here>. There’s a whole lot I can say about this topic beyond just about guzzling water— but the take-away is it’s about giving your body what it needs to use that water effectively.
3. Magnesium Citrate and Triphala
Amy’s stool patterns suggested that her system needed a little extra help. Enter magnesium citrate, a gentle stool softener, and triphala, an Ayurvedic herbal blend known for supporting regularity.
These additions weren’t harsh or disruptive, but they worked quietly in the background to help restore rhythm to her digestion.
When we looked closer at Amy’s bowel habits, it was clear her system needed some additional support to get things moving.
My first stop is usually magnesium citrate —a form of magnesium known for its ability to draw water into the intestines, softening stool and promoting motility without being overly harsh.
Not only does magnesium play a vital role in muscle relaxation (including the smooth muscles of the GI tract), but it also supports hundreds of enzymatic processes – so it's a win-win situation.
Alongside this, we introduced triphala, an ancient Ayurvedic blend of three fruits (amalaki, bibhitaki, and haritaki) that gently supports digestion and elimination. Unlike traditional laxatives, triphala works holistically, helping to tone the digestive tract over time while also offering antioxidant and anti-inflammatory benefits without developing tolerance like senna.
4. Stress, the Vagus Nerve, and the MMC
As we dug deeper into Amy’s daily habits, it became clear that her hectic lifestyle was working against her digestion.
She often ate while multitasking—answering emails, scrolling on her phone, or rushing through meals in between work calls. Barely chewing her food before swallowing. So many of my clients (myself included!) are guilty of these mindless eating habits. .
We began with mindful eating practices: slowing down, chewing thoroughly, and pausing between bites. But there was another critical piece of the puzzle—the vagus nerve.
The vagus nerve acts like a two-way superhighway between the brain and gut, regulating digestion, mood, and inflammation. When activated, it triggers the rest-and-digest state (AKA the parasympathetic system), helping the digestive system do its job.
Chronic stress, however, suppresses this system, keeping the body in a constant state of “fight or flight” (AKA the sympathetic system). When activated, this stress state prevents our nervous system from fully relaxing and allows us to digest our food leading to various gut issues and food reactivities.
To stimulate her vagus nerve, I introduced simple but powerful evidence-based techniques:
- Deep Breathing: Slow, diaphragmatic breathing helps activate the vagus nerve and signal the body to shift into a relaxed state, preparing the digestive system for its work.
- Humming and Gargling: Both techniques stimulate the vagus nerve via vibration, helping to tone and strengthen its function over time. These simple practices can easily be incorporated into a daily routine.
- Neck Stretches: The vagus nerve runs along the neck, and certain stretches can release tension and improve its activation. One effective movement involves tilting the head to one side, holding the stretch for 15–20 seconds, then switching to the other side. Another involves looking over one shoulder and holding for a count, then repeating on the opposite side. These stretches not only support vagus nerve function but also relieve physical tension that accumulates with stress.
Another critical piece of the digestive puzzle is the migrating motor complex (MMC)—a natural cleansing wave that moves undigested food and debris through the gut between meals – like a digestive custodial crew.
Amy’s tendency to graze throughout the day then eat a large, late dinner was disrupting this critical process. By spacing meals 3–4 hours apart, the MMC can activate properly, reducing bloating and promoting smoother digestion.
Together, these strategies address the often-overlooked connection between the nervous system and the gut. Practices like mindful eating, vagus nerve stimulation, and meal timing have been shown to enhance digestive function, reduce bloating, and promote regular bowel movements.
5. Movement, Massage, and Posture
Movement is a well-documented way to improve digestion. Research shows that even light physical activity, such as a 15-minute walk after meals, can stimulate the MMC.
In addition to walking, abdominal massage techniques were introduced to support motility and ease discomfort. These techniques involve applying gentle, clockwise pressure along the path of the colon, starting from the lower right abdomen, moving upward toward the ribs, across to the left side, and then down toward the pelvis. Studies suggest that regular abdominal massage can improve stool consistency and ease symptoms of constipation.
Finally, we addressed posture during bowel movements. A standard seated position on a toilet often creates an angle that can make elimination more difficult. Incorporating a Squatty Potty—a footstool designed to elevate the legs and mimic a squatting position—helped align the rectum for easier, more complete bowel movements. This simple change in positioning can reduce straining and improve overall bowel health.
Important Tip: Avoid sitting on the toilet for too long! If you can’t go, don’t sit there and just doom scroll away on your phone (common, we all do it, but seriously it’s a bad habit). This can lead to unnecessary strain, increasing the risk of hemorrhoids, weaken the pelvic muscles, or cause a rectal prolapse.
The Detective Work That Made the Difference
For Amy, constipation wasn’t at the top of her list of concerns. She had lived with it for so long that it simply felt normal.
I see this all the time, and for what it’s worth, there’s zero judgment here. Many of us don’t immediately recognize the connections between our symptoms—until someone helps us piece them together.
And that’s exactly why it stood out during our assessment. Chronic constipation is more than an inconvenience; it’s often a red flag that both influences and is influenced by a long list of other symptoms. In Amy’s case, her sluggish digestion was quietly contributing to hormone dysregulation, low energy, and even her severe PMS symptoms.
By doing a little digging into her symptoms, habits, and history, we uncovered how her gut health was a missing link in her overall wellness. Addressing her constipation wasn’t just about improving bowel habits; it became the foundation for better hormone balance, clearer thinking, and more sustainable energy.
Sometimes, the seemingly “normal” things we brush off hold the biggest clues to unlocking major transformations.
The Results: A Ripple Effect of Health Improvements
Within weeks, Amy’s digestion started to improve. Her bowel movements became regular, easier to pass, and less of an ordeal. But the changes didn’t stop there—what truly surprised her was how better digestion had a ripple effect on the rest of her health.
Her PMS symptoms were the first to shift. The headaches that had sidelined her for days were less frequent, and while she still felt tired before her period, it was manageable—no longer the all-consuming fatigue she’d come to dread. These small wins were proof that her body was starting to respond.
While her hormones, allergies, and histamine issues required more focused interventions (more on that in a future post), Amy made an impactful connection: tackling her gut health was about creating a foundation for habits that supported her entire body.
Ending Constipation: A Digestive Health Toolkit
Addressing constipation and improving gut health requires a thoughtful balance of diet, supplements, and lifestyle. Here’s how to lay a strong foundation:
Foods That Support Motility: Incorporate these gut-friendly options:
- Prunes: Containing natural sorbitol, prunes gently stimulate the bowels. Eat 2–3 daily or add to smoothies.
- Chia Seeds: Soak 1–2 tablespoons in water or almond milk for a gel-like pudding that promotes stool formation.
- Flaxseeds: Ground flaxseeds provide soluble fiber and omega-3s. Add a tablespoon to oatmeal, yogurt, or salads daily.
- Kiwi: Studies show 1–2 kiwis per day improve motility and ease constipation.
Choose Fiber Wisely: If fiber or probiotics seem to worsen symptoms like bloating or discomfort, this might indicate underlying issues such as SIBO (small intestinal bacterial overgrowth) or dysbiosis. While elimination diets like low-FODMAP can temporarily help reduce symptoms, they’re not a long-term solution. If this resonates with your experience, consider consulting a professional to explore root causes and personalized interventions.
Hydration is Key: Staying hydrated is essential for motility, but it’s more than just drinking water. Aim for steady hydration throughout the day, and include hydrating foods like cucumber, citrus fruits, and soups. Proper hydration helps soften stool and supports the gut’s ability to move waste effectively.
Feed the Microbiome Thoughtfully: Focus on “safe” microbiome-friendly foods that won’t exacerbate bloating. These include a variety of cooked, colorful vegetables (like carrots, pumpkin, and Swiss chard), low-FODMAP fruits (such as kiwi, berries, and papaya), and anti-inflammatory options like turmeric and ginger. Polyphenol-rich foods like pomegranate seeds, dark chocolate, green tea, and extra virgin olive oil support microbial diversity and overall gut health.
Download your FREE rainbow evaluation HERE
Supplements: Gentle and Targeted Support
Magnesium Citrate: Take 200–400 mg in the evening with water to support regularity. Start with a lower dose and increase gradually, as needed, to avoid loose stools.
Triphala: Take 1–2 capsules or 1 teaspoon of powder mixed with warm water before bed to gently support digestion and regular bowel movements.
Digestive Bitters: Use 1–2 droppers of bitters (or follow the product’s dosage); can be taken 10–15 minutes before meals or taken between meals to promote better digestion motility. Hold the bitters on your tongue briefly to stimulate digestive secretions, then swallow.
Prokinetic Agents: For sluggish digestion, try natural options like ginger tea after meals or supplements containing ginger, artichoke, or motility-support herbs.
Electrolytes: Mix a clean electrolyte formula, like LMNT or Redmonds ReLyte, into a glass of water once or twice daily. Alternatively, add a pinch of sea salt and a squeeze of lemon to your water for a homemade option.
View my comprehensive constipation protocol HERE***
***Create a Fullscript account to view
Lifestyle Practices: Set the Stage for Digestion
Abdominal Massage: Gently massage your abdomen in a clockwise direction, following the path of the colon. Start at the lower right, move up toward your ribs, across to the left side, and then down toward your pelvis. This helps stimulate motility and ease constipation.
Vagal Nerve Activation: Engage your parasympathetic nervous system to support digestion:
Practice diaphragmatic breathing—slow, deep breaths into your belly.
Try neck stretches, tilting your head side to side and holding each stretch for 15–20 seconds to relieve tension along the vagus nerve.
Incorporate humming or gargling for 30–60 seconds daily to stimulate vagus nerve function.
Mindful Eating: Chew your food thoroughly, breathe deeply before meals, and avoid eating on the go to promote the “rest-and-digest” state.
Leverage the MMC: A 3–4 hour gap between meals and before bedtime is ideal for supporting this natural process.
Move After Meals: A simple 15-minute walk after eating can stimulate digestion and reduce bloating.
Use a Squatty Potty: Elevate your feet during bowel movements to align your rectum and allow for easier, strain-free elimination.
The Takeaway
Constipation is so common it’s become one of those things many of us brush off or normalize. But as I hope Amy’s story shows, addressing something as basic as digestion can lead to a ripple effect.
Amy noted improvements in her energy and hormones, Improved digestion also means she’s getting more from her diet – she’s actually absorbing nutrients and nourishing her body. But there’s also a subtle impact, the habits she’s building are essential for any other steps she’s going to adopt for the deeper dives into her hormones and allergy symptoms.
If you relate to Amy’s story, and you’re ready to stop the rollercoaster of symptoms and start making real progress, begin with the strategies outlined here.
And remember, you don’t have to figure it all out on your own.
I specialize in helping clients connect the dots, uncover the root causes of their symptoms, and build personalized, realistic plans that actually work. Together, we can uncover the root causes of your symptoms and build a plan tailored to your needs.
👉 Learn about programs and consultation options
Top 12 Supplements for Blood Sugar Control: Backed by Research
The foundation of blood sugar regulation starts with diet and lifestyle. Managing macronutrient balance, prioritizing diet quality, and incorporating regular movement are essential first steps. These strategies lay the groundwork for steady blood sugar levels and improved metabolic health.
However, blood sugar regulation is a complex process influenced by deeper factors like inflammation, insulin sensitivity, and gut health. (For a deep dive into these connections, check out our comprehensive blog on the relationship between blood sugar, inflammation, and the microbiome.)
In many cases, nutrient depletions, increased metabolic demands, and/or specific health conditions can leave the body needing additional support. This is where nutraceuticals (herbs, nutrients, and other targeted supplements) can play a pivotal role. By addressing root causes and filling in the gaps, they work alongside diet and lifestyle changes to enhance results, improve insulin sensitivity, and reduce fasting glucose.
In this blog, we’ll explore the 12 most effective supplements for balancing blood sugar, with evidence-based mechanisms, dosing tips, and clinical applications to help you make informed choices.
1. Berberine
Why It Works:
Berberine is often called “nature’s metformin,” and for good reason. It activates AMPK, a key enzyme in energy metabolism, which helps reduce liver glucose production and improve insulin sensitivity. Research has shown that berberine can lower HbA1c levels by ~1%, a result comparable to metformin.
Dose and Clinical Tips:
- Dose: 500 mg, 2–3x/day with meals (target 1000 - 2000mg/day).
- Tip: Take with food to minimize gastrointestinal discomfort
2. Magnesium
Why It Works:
Magnesium is crucial for insulin function and glucose metabolism, yet magnesium deficiency is common in individuals with insulin resistance. Studies show supplementation improves fasting glucose and insulin sensitivity, particularly in magnesium-deficient individuals. Magnesium also improves levels of circulating vitamin D, another important nutrient in blood sugar control.
Dose and Clinical Tips:
- Dose: 200–400 mg/day.
- Forms: Magnesium glycinate or malate are preferred for better absorption, specific metabolic benefits, and reduced GI side effects. Avoid magnesium oxide, which is poorly absorbed.
3. Omega-3 Fatty Acids
Why It Works:
Omega-3s reduce systemic inflammation, a key driver of insulin resistance and metabolic dysfunction. They also improve lipid profiles and reduce triglyceride levels, which are often elevated in those with poor blood sugar control.
Dose and Clinical Tips:
- Dose: 2–4 g/day of combined EPA/DHA.
- Quality Tip: When choosing an omega-3 supplement, prioritize molecularly distilled fish oil or algae-based alternatives to ensure purity. Triglyceride (TG) forms are considered better absorbed over ethyl ester forms. High-quality fish oil should also be third party tested for rancidity—oxidized oils can lose effectiveness and may even promote inflammation – and screened for heavy metals like mercury. Remember, a high-quality fish oil supplement won’t cause the dreaded “fish burps,” a sign of lower quality or poor formulation.
4. Vitamin D
Why It Works:
Vitamin D plays a vital role in regulating insulin secretion and improving sensitivity. Low vitamin D levels are linked to increased insulin resistance and poor glucose metabolism, as well as increased risk of cardiovascular complications. Optimizing vitamin D levels can improve all of these outcomes. Regular blood testing to monitor levels and adjust dose accordingly is the ideal method for achieving a personalized target dose.
Dose and Clinical Tips:
- Dose: generally 2,000–5,000 IU/day.
- Forms: D3 paired with K2 enhances absorption and supports calcium metabolism. Aim for serum levels of 50+ ng/mL. Magnesium deficiency will interfere with vitamin D optimization.
5. Alpha-Lipoic Acid (ALA)
Why It Works:
ALA is a powerful antioxidant that improves insulin sensitivity, supports mitochondrial function, and reduces oxidative stress. It’s particularly beneficial for individuals with fatty liver—a condition closely tied to insulin resistance. Fatty liver impairs glucose regulation by increasing hepatic glucose output and worsening inflammation..
Dose and Clinical Tips:
- Dose: 300–600 mg/day.
- Tip: Take with food or at the same time as fish oil and vitamin D to improve absorption.
6. Probiotics
Broad Spectrum Probiotics
Why They Work:
The gut microbiome plays a critical role in blood sugar regulation. Probiotics improve gut barrier integrity, reduce inflammation, and modulate glucose metabolism. Multi-strain probiotics containing Lactobacillus and Bifidobacterium species are particularly effective according to studies.
Dose and Clinical Tips:
- Dose: Varies; generally starts at 10–20 billion CFUs/day.
- Tip: Choose high-quality probiotics that guarantee live cultures through expiration.
Akkermansia muciniphila (Strain-Specific Probiotic)
Akkermansia muciniphila is a keystone species in the gut microbiome, playing a critical role in maintaining gut barrier integrity and regulating metabolic health. Studies have shown that robust levels of Akkermansia are associated with improved insulin sensitivity, lower fasting insulin levels, and reduced systemic inflammation. These effects make it a promising target for managing blood sugar and metabolic disorders like type 2 diabetes and metabolic syndrome.
This bacterium works by enhancing the production of mucin, which supports the gut lining, reducing gut permeability (commonly referred to as “leaky gut”). A healthy gut barrier helps to mitigate systemic inflammation and improve metabolic outcomes, as inflammation is a major driver of insulin resistance. It’s worth noting that excess Akkermansia has been associated with inflammation and leaky gut, so balance is key.
Dose and Clinical Tips:
- Support with: Targeted Akkermansia probiotics or a specific polyphenol blend (derived from berries, pomegranates, green tea) which encourages the growth of Akkermansia in the gut.
- Clinical Tip: Consider stool testing to assess baseline Akkermansia levels and monitor progress. For patients who are low, dietary strategies combined with supplementation can optimize outcomes without promoting excess mucosal irritation.
7. Fiber (Dietary and Supplemental)
Dietary fiber is essential for gut health and blood sugar regulation. Soluble fibers, in particular, slow glucose absorption, stabilize blood sugar levels, and serve as a fuel source for beneficial gut bacteria. These bacteria ferment fiber to produce short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate, which play a critical role in metabolic health by improving gut barrier integrity, reducing inflammation, and enhancing insulin sensitivity.
Key Fibers to Include:
- Hydrolyzed Guar Gum (PHGG): A soluble fiber derived from guar beans, PHGG is gentle on the gut and well-tolerated even in those with digestive sensitivities. It promotes SCFA production and improves glycemic control by slowing glucose absorption.
- Pectin: Found in apples, citrus fruits, and berries, pectin is a soluble fiber that feeds beneficial gut bacteria and helps regulate postprandial blood sugar levels.
- Arabinogalactan: A prebiotic fiber derived from larch trees, arabinogalactan promotes the growth of Lactobacillus and Bifidobacterium species, enhances immune function, and supports the gut microbiome’s role in blood sugar regulation.
- Inulin and Fructooligosaccharides (FOS): Found in chicory root, garlic, onions, and bananas, these fibers specifically encourage the growth of beneficial bacteria like Bifidobacterium and increase SCFA production.
- Resistant Starch: Found in cooled, cooked potatoes, green bananas, and legumes, resistant starch improves insulin sensitivity and enhances gut health by feeding butyrate-producing bacteria.
Why Avoid Synthetic Fibers?
While synthetic fibers like those found in many commercial laxatives (e.g., psyllium husk in Metamucil) can provide some benefit, they often lack the diverse prebiotic activity of natural fibers. Synthetic formulations are typically isolated, not well-fermented by the microbiome, and may not support SCFA production as effectively as whole or naturally derived fibers.
Clinical Tips:
- Start Slowly: Gradually increase fiber intake to 25–35 g/day to minimize bloating or discomfort.
- Stay Hydrated: Drink plenty of water to support digestion and prevent GI distress.
- Prioritize Variety: Incorporating a range of fiber types supports a more diverse gut microbiome and maximizes metabolic benefits.
8. Chromium
Why It Works:
Chromium is a trace mineral with a big impact on blood sugar control. It enhances insulin receptor activity, making cells more responsive to insulin, which improves glucose uptake and reduces fasting blood sugar levels. This makes chromium particularly effective for individuals struggling with poorly controlled blood sugar or insulin resistance.
Studies have shown that chromium supplementation can significantly lower HbA1c and fasting glucose, especially in those with type 2 diabetes or metabolic syndrome. By optimizing how the body uses insulin, chromium helps break the cycle of elevated glucose and insulin resistance, supporting more stable energy levels and improved metabolic health.
Dose and Clinical Tips:
- Dose: 200–1,000 µg/day (picolinate form).
- Tip: Take with meals to maximize effectiveness.
9. Cinnamon Extract
Why It Works:
Cinnamon is a traditional herb known for its impact on blood sugar control. It enhances insulin sensitivity and boosts glucose uptake by activating insulin receptors, helping cells use glucose more efficiently.
Beyond its glucose-lowering effects, cinnamon also has antioxidant properties that combat oxidative stress, further supporting metabolic health.
Dose and Clinical Tips:
- Dose: 1–6 g/day of cinnamon extract.
- Tip: Choose Ceylon cinnamon to reduce the risk of liver toxicity from coumarin found in cassia varieties.
10. Curcumin
Why It Works:
Curcumin is the vibrant active compound in turmeric. It also reduces inflammation and oxidative stress—two major drivers of insulin resistance—while directly improving insulin sensitivity.
What sets curcumin apart is its ability to support pancreatic beta-cell function, which is critical for producing and regulating insulin. By protecting these cells from inflammatory damage, curcumin not only helps stabilize blood sugar but also supports long-term metabolic health.
Dose and Clinical Tips:
- Dose: 500–2,000 mg/day.
- Tip: Combine with piperine (black pepper extract) to enhance absorption by up to 2,000%.
11. Green Tea Extract (EGCG)
Why It Works:
EGCG is the powerful antioxidant and polyphenol found in green tea. It’s one of the most well studied compounds for metabolic health. It has been shown to improve glucose metabolism by enhancing insulin sensitivity and reducing inflammatory markers—both critical factors in blood sugar regulation.
Beyond its effects on glucose control, EGCG also boosts fat oxidation, making it a valuable tool for supporting weight management and reducing visceral fat, a key driver of insulin resistance. Furthermore, EGCG is known to enhance the favorable microbiome environment associated with improved metabolism. Its anti-inflammatory and antioxidant properties make EGCG a multifaceted nutraceutical for improving overall metabolic health.
Dose and Clinical Tips:
- Dose: 400–800 mg/day.
- Tip: Tannins in tea, including EGCG, can bind with non-heme iron, forming insoluble complexes that reduce its bioavailability. Avoid taking it with iron-rich meals to prevent reduced bioavailability.
12. Resveratrol
Why It Works:
Resveratrol, a potent polyphenol found in red grapes, berries, and other red and orange foods, is a metabolic game-changer. It activates AMPK, a key enzyme involved in energy regulation, to enhance insulin sensitivity and lower fasting glucose levels.
What makes resveratrol particularly powerful is its dual action: alongside improving glucose metabolism, it delivers potent anti-inflammatory effects, helping to combat the chronic inflammation that drives insulin resistance and metabolic dysfunction. This unique combination makes resveratrol a valuable ally in improving blood sugar and supporting long-term metabolic health.
Dose and Clinical Tips:
- Dose: 500–1,000 mg/day.
- Tip: Combine with a diet rich in polyphenols for synergistic benefits.
Conclusion: A note on synergy for better blood sugar control
The foundation of blood sugar regulation always begins with diet and lifestyle. A nutrient-dense, balanced diet combined with regular movement is essential for improving metabolic health, managing inflammation, and stabilizing blood sugar levels. These are the cornerstones of any effective approach which supplements cannot replace.
Herbs and nutritional compounds provide a unique advantage by working synergistically with the body’s natural systems. Unlike pharmaceuticals, which often target a single pathway, nutraceuticals offer a more balanced approach, addressing multiple underlying factors such as inflammation, oxidative stress, microbiome balance, and insulin sensitivity simultaneously.
It’s important to note that this list isn’t exhaustive, nor are we suggesting that everyone needs to take all of these supplements. The right approach emphasizes personalization. The right combination of supplements should be carefully curated based on individual needs, metabolic markers, confounding factors, and health goals.
Diet, lifestyle, and targeted nutraceuticals create a holistic framework for long-term health—not just by managing symptoms but by addressing the root causes of dysregulation.
Curious how your diet supports your metabolic health? Download the free Rainbow Evaluation to assess your plant diversity and start optimizing your blood sugar control today!
References
- Dama A, Shpati K, Daliu P, Dumur S, Gorica E, Santini A. Targeting Metabolic Diseases: The Role of Nutraceuticals in Modulating Oxidative Stress and Inflammation. Nutrients. 2024;16(4):507. Published 2024 Feb 10. doi:10.3390/nu16040507. https://pmc.ncbi.nlm.nih.gov/articles/PMC10891887/
- Wang, C., Yen, H., Lu, W., Ho, H., Lin, W., Kuo, Y., Huang, Y., Tsai, S., & Lin, H. (2022). Adjuvant Probiotics of Lactobacillus salivarius subsp. salicinius AP-32, L. johnsonii MH-68, and Bifidobacterium animalis subsp. lactis CP-9 Attenuate Glycemic Levels and Inflammatory Cytokines in Patients With Type 1 Diabetes Mellitus. Frontiers in Endocrinology, 13. https://doi.org/10.3389/fendo.2022.754401.
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes. Metabolism. 2008;57(5):712-717. https://pubmed.ncbi.nlm.nih.gov/23118793
- Barbagallo M, Dominguez LJ. Magnesium and type 2 diabetes. Magnesium Research. 2007;20(4):245-252. https://pubmed.ncbi.nlm.nih.gov/12663588
- Bhat S, Sowmya S, Baskaran V, et al. Omega-3 fatty acids and metabolic health. Advances in Nutrition. 2016;7(5):804-818. https://pubmed.ncbi.nlm.nih.gov/27329332
- Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinology and Metabolism Clinics of North America. 2014;43(1):205-232. https://pubmed.ncbi.nlm.nih.gov/27528514
- Henriksen EJ, Diamond-Stanic MK. Modulation of insulin resistance and glucose tolerance by alpha-lipoic acid. Current Pharmaceutical Design. 2011;17(33):3948-3958. https://pubmed.ncbi.nlm.nih.gov/15263922
- Depommier C, Everard A, Druart C, et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: A proof-of-concept exploratory study. Nat Med. 2019;25(7):1096-1103. https://doi.org/10.1038/s41591-019-0495-2
- Canfora E, Jocken J, Blaak E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. 2015;11:577-591. https://doi.org/10.1038/nrendo.2015.128
- Asbaghi O, Choghakhori R, Sadeghian M, et al. Effects of chromium supplementation on glycemic control in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Journal of Trace Elements in Medicine and Biology. 2020;62:126603. https://pubmed.ncbi.nlm.nih.gov/32687991
- Khan A, Safdar M, Khan MMA, et al. Cinnamon improves glucose and lipids of people with type 2 diabetes. Am J Clin Nutr. 2003;78(4):725-732. https://pubmed.ncbi.nlm.nih.gov/14633804/
- Na L, Li X. Curcuminoids exert glucose-lowering effect in type 2 diabetes through multiple mechanisms. Pharmacol Res. 2013;76:8-12. https://doi.org/10.1016/j.phrs.2017.09.010
- Hsu CH, Liao YL. Does supplementation with green tea extract improve glucose regulation and insulin sensitivity in obese individuals with type 2 diabetes? Obes Res Clin Pract. 2011;5(4):e267-e348. https://pubmed.ncbi.nlm.nih.gov/27329332
- Movahed A, Nabipour I, Louis XL, et al. Antihyperglycemic effects of short-term resveratrol supplementation in type 2 diabetic patients: A randomized placebo-controlled study. PLoS One. 2013;8(7):e70360. https://doi.org/10.1155/2013/851267
- Weisberg, S., Leibel, R., & Tortoriello, D. (2016). Proteasome inhibitors, including curcumin, improve pancreatic β-cell function and insulin sensitivity in diabetic mice. Nutrition & Diabetes, 6. https://doi.org/10.1038/nutd.2016.13
- Delimont, N., Haub, M., & Lindshield, B. (2017). The Impact of Tannin Consumption on Iron Bioavailability and Status: A Narrative Review. Current Developments in Nutrition, 1, 1 - 12. https://doi.org/10.3945/cdn.116.000042










