Natural Solutions for Histamine Intolerance: A Root-Cause Approach
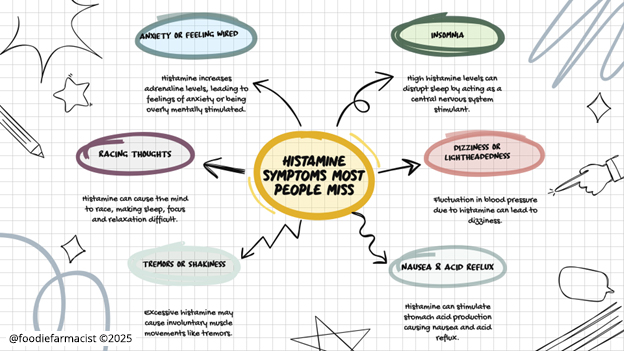
If you’ve been struggling with histamine-related symptoms—bloating, headaches, anxiety, PMS, or skin flare-ups—you’ve probably tried everything from food eliminations to antihistamines like Pepcid or Zyrtec.
These strategies might help in the short term, but they don’t fix the deeper issue: the root cause of why your body is struggling to break down histamine in the first place.
A true root-cause approach looks beyond symptom management and focuses on supporting histamine metabolism, gut health, and hormone balance so your body can regulate histamine naturally.
How to Naturally Support Histamine Clearance
Your body has built-in systems to break down histamine efficiently—but only when those systems are working properly. The key to long-term relief is supporting:
- Enzymes that break down histamine (like DAO and HNMT)
- The gut microbiome (to prevent histamine buildup and estrogen recirculation)
- Liver detox pathways (to clear histamine and estrogen effectively)
- Nutrients that regulate histamine production and inflammation
Here’s where to start:
1. Nutrients That Support Histamine Breakdown
Your body relies on specific enzymes—diamine oxidase (DAO) and histamine-N-methyltransferase (HNMT)—to break down histamine. If these enzymes aren’t working efficiently, histamine builds up, leading to symptoms.
These nutrients help:
- Vitamin C – A natural antihistamine that stabilizes mast cells and reduces histamine release. Found in bell peppers, citrus fruits, and kiwi.
- Vitamin B6 – Supports DAO enzyme production, which helps clear histamine from the body. Found in bananas, poultry, and sunflower seeds.
- Magnesium – Helps regulate histamine metabolism and prevent overproduction. Found in leafy greens, nuts, and seeds.
2. Herbs and Polyphenols That Stabilize Mast Cells
Mast cells release histamine as part of an immune response, but in histamine intolerance, they can become overactive. Certain plant compounds can help stabilize mast cells and reduce excessive histamine release.
- Quercetin – A potent flavonoid that helps stabilize mast cells and reduce inflammation. Found in apples, onions, and capers.
- Stinging Nettle – Traditionally used for allergies, nettle inhibits histamine release and supports immune balance.
- Curcumin – Found in turmeric, curcumin has anti-inflammatory and mast-cell stabilizing properties.
3. Gut-Supportive Compounds
Since the gut microbiome plays a major role in histamine metabolism, supporting gut health is essential for reducing histamine intolerance.
- Probiotics (Carefully Chosen) – Not all probiotics are beneficial for histamine intolerance. Look for strains like Bifidobacterium infantis and Lactobacillus plantarum, which help regulate histamine without increasing its production.
- Prebiotic Fibers –Foods like artichokes, asparagus, and green bananas feed beneficial gut bacteria and support DAO production.
- Glutamine – Helps heal the gut lining and reduce inflammation that can trigger histamine release.
4. Liver Detox Support
Your liver is responsible for clearing both histamine and excess estrogen. If detox pathways are sluggish, histamine can build up in the body.
- Sulfur-Rich Vegetables – Cruciferous veggies like broccoli, cabbage, and Brussels sprouts support estrogen and histamine metabolism.
- Milk Thistle – Supports liver detox and helps eliminate excess histamine and estrogen.
- Dandelion Root – A gentle liver tonic that promotes bile flow and estrogen clearance.
A Holistic Approach for Long-Term Relief
Managing histamine intolerance isn’t about avoiding high-histamine foods forever or relying on antihistamines. It’s about giving your body the tools it needs to regulate histamine naturally.
The right nutrients, gut support, and hormone balance strategies can help reduce histamine symptoms while addressing the root causes—so you can finally feel better.
Want a step-by-step plan?
📥 Download the full Estrogen + Histamine Guide here →
Inside, you’ll find a comprehensive approach to histamine intolerance, including food strategies, supplements, and practical tools to support your body naturally.
References:
- Fiorani M, Del Vecchio LE, Dargenio P, et al. Histamine-producing bacteria and their role in gastrointestinal disorders. Expert Rev Gastroenterol Hepatol. 2023;17(7):709-718. doi:10.1080/17474124.2023.2230865.
https://doi.org/10.1080/17474124.2023.2230865 - Khan M, Khan ZA, Naeem A, et al. Effect of dietary modification for targeting histamine activity in patients of allergic rhinitis: a randomized open-label study. Research Square. Published 2020. doi:10.21203/rs.3.rs-25717/v1.
https://doi.org/10.21203/rs.3.rs-25717/v1 - Cao M, Gao Y. Mast cell stabilizers: from pathogenic roles to targeting therapies. Front Immunol. 2024;15:1418897. Published August 1, 2024. doi:10.3389/fimmu.2024.1418897.
https://doi.org/10.3389/fimmu.2024.1418897 - Zeng J, Hao J, Yang Z, et al. Anti-allergic effect of dietary polyphenols curcumin and epigallocatechin gallate via anti-degranulation in IgE/antigen-stimulated mast cell model: A lipidomics perspective. Metabolites. 2023;13(5):628. Published May 5, 2023. doi:10.3390/metabo13050628.
https://doi.org/10.3390/metabo13050628 - Cheng W, Lu J, Li B, et al. Effect of functional oligosaccharides and ordinary dietary fiber on intestinal microbiota diversity. Front Microbiol. 2017;8:1750. Published September 20, 2017. doi:10.3389/fmicb.2017.01750.
https://doi.org/10.3389/fmicb.2017.01750 - Basnet J, Eissa MA, Cardozo LLY, Romero DG, Rezq S. Impact of probiotics and prebiotics on gut microbiome and hormonal regulation. Gastrointest Disord. 2024;6(4):801-815. doi:10.3390/gidisord6040056.
https://doi.org/10.3390/gidisord6040056
Can Your Gut Make You Histamine Intolerant? The Microbiome-Histamine Connection
If you have been dealing with histamine intolerance, you have likely been told to focus on avoiding high-histamine foods. While diet plays a role, histamine overload is not just about what you eat—it is about how your body processes and eliminates histamine.
Why Gut Health Is the Missing Piece in Histamine Intolerance
Your gut microbiome is one of the most important regulators of histamine metabolism. If your digestion is sluggish, your gut bacteria is out of balance, or your intestinal barrier is compromised, histamine intolerance can become significantly worse.
If you experience histamine-related symptoms such as bloating, nausea, acid reflux, skin rashes, or headaches, your gut may be driving the problem.
Let’s break down how the microbiome impacts histamine levels—and what you can do to fix it.
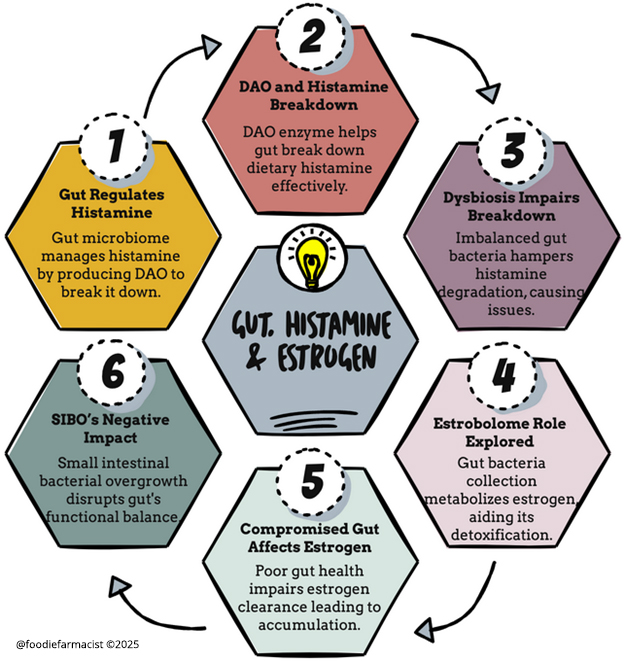
How the Gut Regulates Histamine
Histamine is produced and broken down in multiple areas of the body, but the gut is one of the primary control centers. There are three main ways your gut impacts histamine levels:
1. Certain Gut Bacteria Produce Histamine
Some gut bacteria naturally produce histamine as part of their metabolism. If these histamine-producing bacteria overgrow, histamine levels in the body can rise, leading to symptoms such as bloating, headaches, and flushing.
- Histamine-producing bacteria include:
- Morganella morganii
- Klebsiella pneumoniae
- Escherichia coli (certain strains)
If your microbiome is imbalanced—whether due to dysbiosis, SIBO (small intestinal bacterial overgrowth), or low gut diversity—you may have more histamine-producing bacteria than histamine-degrading ones. Stool testing through companies like DSL GI Map can help identify these imbalances.
2. The Gut Produces DAO (The Histamine-Breaking Enzyme)
DAO (diamine oxidase) is the main enzyme responsible for breaking down histamine from food. It is produced in the gut lining, which means that if gut health is compromised, DAO production may decline.
Factors that can reduce DAO production include:
- Leaky gut (intestinal permeability)
- Chronic inflammation or gut infections
- Food sensitivities that trigger gut irritation
- Certain medications (such as NSAIDs and proton pump inhibitors)
If DAO levels are too low, even a small amount of histamine from food can trigger symptoms.
3. The Gut Helps Eliminate Excess Histamine and Estrogen
Your gut microbiome also plays a crucial role in estrogen metabolism. The estrobolome (a subset of gut bacteria) helps break down and eliminate estrogen. If this process is disrupted, estrogen can recirculate in the body, further increasing histamine levels.
This means that if you have histamine intolerance and your digestion is slow or your microbiome is out of balance, you may also be holding onto excess estrogen—which can further fuel the histamine cycle.
Why Some Probiotics Can Make Histamine Intolerance Worse
Probiotics are often recommended for gut health, but not all probiotics are beneficial for histamine intolerance. Some strains actually produce histamine, which can worsen symptoms.
- Probiotics that may increase histamine:
- Lactobacillus casei
- Lactobacillus bulgaricus
- Lactobacillus reuteri
If you have histamine intolerance, taking the wrong probiotic could actually make symptoms worse, especially if your microbiome is already imbalanced.
The Right Gut-Health Strategies for Histamine Intolerance
Instead of focusing solely on food eliminations, addressing gut health can help regulate histamine metabolism and improve tolerance over time.
1. Support the Gut Lining and DAO Production
- Increase nutrients that support DAO enzyme production, such as vitamin B6, magnesium, and zinc.
- Reduce gut inflammation by avoiding processed foods, alcohol, and excessive caffeine.
- Incorporate gut-healing foods such as bone broth, aloe vera, and glutamine.
2. Focus on Probiotics That Degrade Histamine
Instead of taking general probiotics, focus on strains that help break down histamine rather than produce it.
- Histamine-degrading probiotics include:
- Bifidobacterium infantis
- Bifidobacterium longum
- Lactobacillus plantarum
These strains can help restore microbial balance and improve histamine tolerance over time.
3. Improve Gut Motility and Digestion
- Increase fiber intake from vegetables and flaxseeds to help clear histamine and estrogen.
- Support digestive enzymes and bile flow with bitters, ginger, and dandelion root.
- Hydrate properly to ensure smooth digestion and detoxification.
The Bottom Line
If you are struggling with histamine intolerance, focusing only on food eliminations will not solve the problem. Your gut plays a critical role in how your body processes and eliminates histamine, and if your microbiome is imbalanced, histamine intolerance will persist.
By improving gut health, increasing DAO activity, and choosing the right probiotics, you can build long-term resilience against histamine-related symptoms.
For a full step-by-step plan on managing histamine intolerance through gut health, download the Estrogen + Histamine Guide here.
References:
- Fiorani M, Del Vecchio LE, Dargenio P, et al. Histamine-producing bacteria and their role in gastrointestinal disorders. Expert Rev Gastroenterol Hepatol. 2023;17(7):709-718. doi:10.1080/17474124.2023.2230865
- Engevik K, Edens R, Engevik AC, Engevik MA, Horvath T. Production of histamine by diverse gut bacteria can activate intestinal HRH1 and promote calcium mobilization. Physiology. 2024;39(s1):2142. doi:10.1152/physiol.2024.39.s1.2142
- Mou Z, Yang Y, Hall AB, Jiang X. The taxonomic distribution of histamine-secreting bacteria in the human gut microbiome. BMC Genomics. 2021;22(1):Article 4. doi:10.1186/s12864-021-08004-3
- Smolinska S, Winiarska E, Głobińska A, Jutel M. Histamine: A mediator of intestinal disorders—a review. Metabolites. 2022;12(10):895. doi:10.3390/metabo12100895
- Sánchez-Pérez S, Comas-Basté O, Duelo A, et al. Intestinal dysbiosis in patients with histamine intolerance. Nutrients. 2022;14(9):1774. doi:10.3390/nu14091774
- Kumari N, Kumari R, Dua A, et al. From gut to hormones: Unraveling the role of gut microbiota in (phyto)estrogen modulation in health and disease. Mol Nutr Food Res. 2024;68(6):e2300688. doi:10.1002/mnfr.202300688
- Hu S, Ding Q, Zhang W, Kang M, Ma J, Zhao L. Gut microbial beta-glucuronidase: a vital regulator in female estrogen metabolism. Gut Microbes. 2023;15(1):2236749. doi:10.1080/19490976.2023.2236749
- Barber TM, Kabisch S, Pfeiffer AFH, Weickert MO. The health benefits of dietary fibre. Nutrients. 2020;12(10):3209. Published 2020 Oct 21. doi:10.3390/nu12103209


