Few nutrients have emerged as significant to our overall health as vitamin D – often referred to as the “sunshine vitamin” because we can make it with adequate sunlight exposure. However with our modern lifestyles and concerns surrounding sun damage, we’ve observed a trend of deficiency.
Most of us appreciate the role of the “sunshine vitamin” as aiding calcium in building bone density, but Vitamin D has a diverse set of function beyond bone health, including:
- Immune System Support: Reducing inflammation and improving antimicrobial defense, including reduced risk of complications from influenza and COVID-19
- Autoimmune disease: Reduced risk of autoimmune disease development and relapse including Hoshimotos, Inflammatory Bowel Disease (IBD), rheumatoid arthritis, multiple sclerosis, and psoriasis among others.
- Cardioprotective: Improved risk factors for cardiovascular disease (CVD) including blood pressure regulation, vascular health and flexibility, cholesterol, reduced oxidative stress
- Blood sugar balance: Vitamin D supports insulin production in response to glucose and insulin sensitivity for better glycemic control
- Neuroprotective: Reduces risk of neurodegeneration reduces neurotoxicity due to oxidative damage
- Cancer risk: Reduced cell proliferation, tumor growth, and metastasis
- Musculoskeletal health: support bone mineralization to reduce risk of bone loss and even improves muscle mass and reduces fall risk in those over 65 years-old.
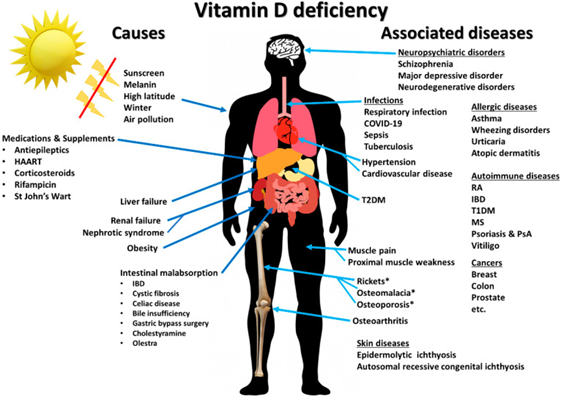
Illustration from https://pubmed.ncbi.nlm.nih.gov/32679784/
Vitamin D actually has hormonal properties that have been associated with sleep-wake cycle – also referred to as circadian rhythm. The”sunshine vitamin” might be related to balancing circadian rhythm by playing a counter role to melatonin – like the ying to its yang.
Significant deficiencies of vitamin D are also associated with Rickets, osteomalacia, and muscle and bone weakness.
I rounded up my favorite vitamin D supplements in a Fullscript protocol. You can find my favorite Vit D forms and dosage options here: https://us.fullscript.com/plans/lzakaria-personalizing-your-vit-d-dose
The road to optimizing vitamin D
Deficiencies of vitamin D are common – in fact, it has been referred to as the vitamin D epidemic. To better understand why it’s been so challenging to pin down the recommendations, let’s review all the factors that result in bioindividual variations.
First a little biochemistry background
Biochemistry not your thing? All good – skip down to sources of vitamin D below.
Cholecalciferol and ergocalciferol, the biologically inactive precursors of vitamin D, are activated by UVB exposure to form calcitriol. The precursors pass through the liver then the kidneys for activation before entering systemic circulation. Vitamin D activation and activity has been associated with a variety of tissues throughout the body, including skin, parathyroid gland, breast, colon, prostate, as well as cells of the immune system and bone cells.
25-Hydroxyvitamin D (25-OH vit D or calcifediol) constitutes the major circulating form of vitamin D (a combination of the total of 25-OH D2 and 25-OH D3 form) and is used to determine the serum concentrations to determine vitamin D nutritional status. Most of the physiological effects of vitamin D in the body are related to the activity of 1α,25-dihydroxyvitamin D (calcitriol).
Vitamin D acts through modulation of a transcription factor known as the vitamin D receptor (VDR). Think of this as a lock with a code, when vitamin D is present it unlocks the activity of VDR which turns on a sequence of genes that is responsible for its activity. This messenger system is why we often refer to vitamin D as a hormone. This transcription factor also requires vitamin A, which is the first example of nutrient synergy required for optimal vitamin D levels.
Sources of vitamin D
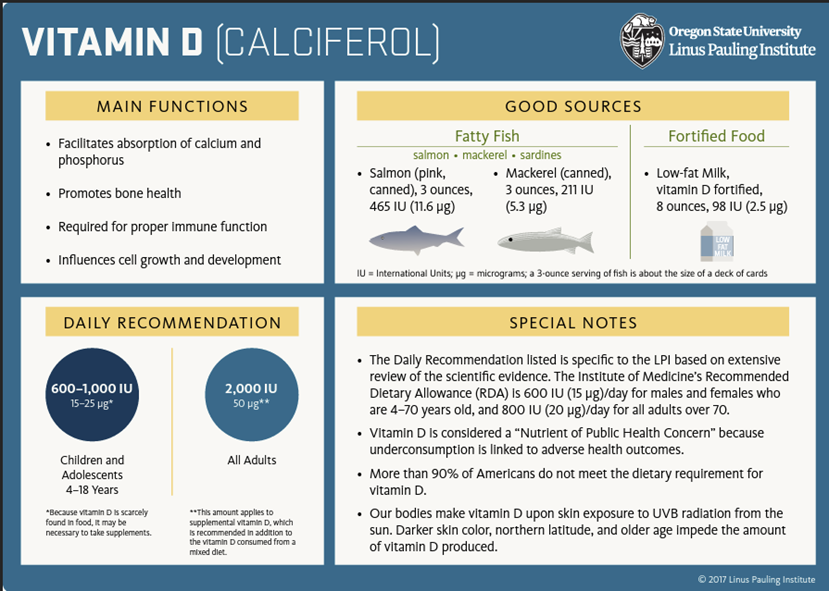
Reprinted with permission from Linus Pauling Institute
Sun exposure is the “gold standard” approach for maximizing vitamin D levels. Recommendations are 15-30 min of daily sun exposure to skin on the arms, torso, and/or legs. It’s been suggested that 15 minutes/day of sun exposure may be the equivalent of 1,000IU of vitamin D supplementation in light skinned individuals (more about this under risk factors below).
Alongside sun exposure, there are some foods that naturally contain vitamin D. These include fatty fish (mackerel, salmon, sardines), fish liver oils, eggs, and animal liver – all great sources of vitamin D3. There’s one significant vegetarian source – mushrooms that have been exposed to sunlight or UV light which produce vitamin D2.
There are also vitamin D fortified foods, meaning they don’t naturally contain significant sources of vitamin D but it’s been added to help fill a public health need. Milk is a great example – where vitamin D isn’t typically found in milk, it’s been fortified to help support calcium absorption.
All that said, it’s challenging to get an accurate estimate of average dietary intakes of vitamin D due to high variability of vitamin D content. You can look up details of the nutrient content of specific foods on USDA’s FoodData Central database.
Defining vitamin D deficiency, insufficiency, and sufficiency
You may have noticed that the reference ranges for vitamin D lab levels vary depending on the lab and that clinicians often have different opinions on targets. That’s because more research is needed to establish definitive parameters for defining the cut-offs for vitamin D deficiency and sufficiency 1,5.
Here’s a summary of what we do know:
- Most would agree that deficiency is defined at a level below < 25 ng/mL
- Levels of 40-60 ng/mL seems to be a reasonable target for immune and metabolic outcomes
- Levels between 30-40 ng/mL are generally considered sufficient for preventing bone loss
- Levels above 100 ng/mL are not recommended and regarded as toxic
Many functional medicine clinicians will target levels between 60-80 ng/mL in an effort to maximize vitamin D. This is often a clinical judgment based on weighing the pros and cons of maximizing vitamin D levels.
Vitamin D levels above 70 ng/mL can be associated with parathyroid hormone suppression, hypercalcemia, and hypercalciuria, but they are rare and there’s no consensus on that level and it might vary individually.
Although, there’s currently not a lot of literature to support this as a public health therapeutic target above 60 ng/mL, this might be a reasonable individualized targeted approach under sufficient medical guidance.
Remember that Vit D is the foundation for immune health. If you want my top “9 Nutrients & Foods for Boosting Immune Health” download, visit https://bit.ly/Foods4Immunity
Risk factors for vitamin D deficiency
There are multiple environmental, social, and biological factors that might increase someone’s risk of vitamin D deficiency or insufficiency. These includes:
- Geographical location: People living in locations with less light exposure, colder climates, or atmospheric conditions (e.g., air pollution, presence of clouds) which reduce UVB rays and therefore, vitamin D production in skin.
- Sun safety measures: These include limiting sun exposure, wearing protective clothing and hats, and applying sunscreens, hinder skin exposure to sunlight.
- Skin pigmentation: People with a darker complexion synthesize less vitamin D with sunlight exposure relative to light-skin individuals.
- Genetic variations: Certain people have VDR variations (called genetic a polymorphism) that alter vitamin D synthesis and activation.
- Clothing style: People who wear more conservative or warmer clothing; for example practicing Muslim women who cover with long sleeves, ankle-length clothes, and a headscarf (hijab or niqab) were at significantly increased risk of vitamin D deficiency (96% had serum 25-OH D concentrations less than 20 ng/mL, and 60% had vitamin D concentrations below 12 ng/mL according to one study).
- Exclusively breast-fed infants: Exclusively breast-fed and do not receive vitamin D supplementation are at high risk for vitamin D deficiency. The American Academy of Pediatrics recommends that all infants be given an oral vitamin D supplement of 400 IU/day
- Older age: Changes in skin composition, metabolism, liver and kidney function reduces capacity to synthesize vitamin D. This risk is elevated in institutionalized adults who are not supplemented with vitamin D.
- Chronic kidney disease (CKD): Reduced kidney activation of vitamin D due to impaired renal function in CKD as well as increased loss of 25-hydroxyvitamin D in urine.
- Increased body mass/altered body composition: Body mass index (BMI) ≥30 kg/m2 increases the risk of vitamin D deficiency because of increased sequestration in body fat stores (reduced bioavailable vitamin D).
- Fat malabsorption: Vitamin D is a fat soluble vitamin, so any condition – including IBD or small bowel resection – that impairs fat absorption will impair vitamin D absorption.
- Magnesium deficiency: Low magnesium is associated with risk of vitamin D deficiency. This is another really significant nutrient synergy for maximizing target levels.
Supplementing Vitamin D
In recent years, the recommendations were changed from an adequate intake (AI) recommendation to a recommended dietary intake (RDA) which is an improvement in recommendations. However, the RDA recommendation is 600-800 IU/day for adults, which most clinicians agree is insufficient to optimize vitamin D levels and continues to contribute to the deficiency epidemic.
There is some research that points to general blood level targets for certain disease states, however, there aren’t currently established dosing recommendations for immune health (or metabolic health, for that matter). However, recent studies suggest between 2000-5000 IU/day are a reasonable target range for most adults to optimize their circulating vitamin D levels.
Supplementing should ideally be the D3 (cholecalciferol) form, most supplements contain this form of the fat soluble vitamin. However, it’s important to note that if you’re taking the prescription version of 50,000 IU vitamin D – often prescribed to be taken once weekly for 12 weeks at initial diagnosis of vitamin D deficiency to quickly raise the levels in circulation – is the D2 (ergocalciferol) precursor.
Here are my thoughts based on my research and clinical experience**:
- Optimal blood levels probably vary individually, 40-60 ng/mL seems to be a reasonable target
- Many of my colleagues – myself included – often aim for 60-80 ng/mL in patients with increased complications of metabolic, autoimmune, and allergic disease. This is still considered reasonably safe below the upper limit of 100 ng/mL. Even though there isn’t any established research to justify this goal this time, it may still be a clinical judgment to personalize targets.
- For most people it’s hard to get enough vitamin D from food and sunshine, especially with the factors discussed above. Therefore, supplementing is usually necessary especially in the winter or if you have darker skin tone.
- Ideally, dosing should be adjusted based on regular monitoring of blood levels and working with a nutritionist or nutrition-savvy clinician. Ideally, I aim for getting a level twice a year if possible – at the lowest level in the early spring, and at the most likely peak in the early Fall.
- I usually start at 2,000-3,000 IU/day (take with food or fish oil to optimize absorption) but frequently will adjust up to 5,000 IU/day to achieve sufficient vitamin D blood levels. I often opt for vitamin D liquid forms (suspended in MCT oil) for best absorption.
- Nutrients often work best in synergy, and vitamin D is no exception. Optimizing the balance of vitamin K2, vitamin A, and magnesium are also important especially if you’re struggling to get to the target blood level. I always work on these before I maximize the vitamin D dose alone.
If you’re looking for resources to help you optimize your vitamin D level, I’ve created a free download you can use as an educational tool that you can bring to your doctor to help you work together to find your optimal vitamin D dose.
You can find my favorite Vit D brand shere: https://us.fullscript.com/plans/lzakaria-personalizing-your-vit-d-dose
Conclusion: And a note to clinicians
Recognizing vitamin D’s therapeutic potential within preventing and managing chronic disease and related symptoms that contribute to quality of life is a critical component of lifestyle medicine. Because it has such wide-reaching benefits, it can be an easy first step to nutrition personalization.
Clinicians: Join me on Fullscript
Fullscript is a digital health platform that helps practitioners build better patient relationships through quality supplementation and intuitive tools for treatment adherence — all at no cost. Beyond supplement planning, Fullscript delivers evidence-based resources, ready-made protocols, personalized refill reminders, and more to help sustain optimal health over time.
Practitioners write online supplement plans or dispense supplements in-office, giving patients easy access to high-quality products and education for optimal health. Physicians and other healthcare practitioners can join Fullscript HERE for free.
**Educational purposes only; talk to your doctor or healthcare provider to determine your optimal dose
References
- Rebelos E, Tentolouris N, Jude E. The Role of Vitamin D in Health and Disease: A Narrative Review on the Mechanisms Linking Vitamin D with Disease and the Effects of Supplementation. Drugs. 2023;83(8):665-685. doi:10.1007/s40265-023-01875-8. https://pubmed.ncbi.nlm.nih.gov/37148471/
- Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020;12(7):2097. Published 2020 Jul 15. doi:10.3390/nu12072097. https://pubmed.ncbi.nlm.nih.gov/32679784/
- Wei FL, Li T, Gao QY, et al. Association Between Vitamin D Supplementation and Fall Prevention. Front Endocrinol (Lausanne). 2022;13:919839. Published 2022 Aug 10. doi:10.3389/fendo.2022.919839. https://pubmed.ncbi.nlm.nih.gov/36034418/
- Pludowski P, Holick MF, Grant WB, et al. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125-135. doi:10.1016/j.jsbmb.2017.01.021. https://pubmed.ncbi.nlm.nih.gov/28216084/
- Romano F, Muscogiuri G, Di Benedetto E, et al. Vitamin D and Sleep Regulation: Is there a Role for Vitamin D?. Curr Pharm Des. 2020;26(21):2492-2496. doi:10.2174/1381612826666200310145935. https://pubmed.ncbi.nlm.nih.gov/32156230/
- https://lpi.oregonstate.edu/mic/vitamins/vitamin-D
- Nichols EK, Khatib IM, Aburto NJ, et al. Vitamin D status and determinants of deficiency among non-pregnant Jordanian women of reproductive age. Eur J Clin Nutr. 2012;66(6):751-756. doi:10.1038/ejcn.2012.25. https://pubmed.ncbi.nlm.nih.gov/22415337/
You May Also Like...
Healthy Hair, Skin, and Nails
Healthy Hair, Skin, and Nails: A Nutritional Approach The condition of your hair, skin, and nails (AKA the…
How Good Digestion Can Improve Overall Health
Good Digestion: The Foundation of Good Health So much emerging research has come up recently connecting the integrity…
Stay In Touch!
Join my mailing list to keep up with all the latest nutrition & FxMed learning opportunities



