By Lara Zakaria, PharmD MS CNS CDN IFMCP & Sara Gibbons MS CNS LDN
Supplements Are on the Rise
In recent years, there’s been a noticeable increase in public interest in—and use of—dietary supplements. As more individuals take charge of their health, they turn to natural products and nutraceuticals to help prevent illness and promote overall wellness.
This trend is partly driven by the growing body of research supporting the health benefits of certain herbs, vitamins, and minerals, and the growing public interest in ways to support health and immunity post-COVID-19 pandemic. However, while supplements offer numerous health benefits, they can also pose risks, particularly when interacting with prescription medications.
This blog explores the various types of drug-nutrient interactions (DNI), drug-induced nutrient depletions (DIND), and drug-herb interactions (DHI). By understanding these interactions, individuals and healthcare professionals can learn about common examples of these interactions, their implications for health, and strategies for managing them effectively.
Benefits and Risks of Dietary Supplements
Many people are unaware that certain supplements can interact with medications, leading to adverse effects or reduced effectiveness of the drugs. These interactions fall into three buckets:
- Drug-Herb Interactions (DHI)
- Drug-Nutrient Interactions (DNI)
- Drug-Induced Nutrient Depletions (DIND)
With more people using supplements, there are more opportunities to educate them on how to use these products safely. Supplement-savvy healthcare professionals can play a key role in guiding and advising individuals about safe and effective nutraceutical use, therefore improving overall health outcomes.
How Medications Can Deplete Nutrients
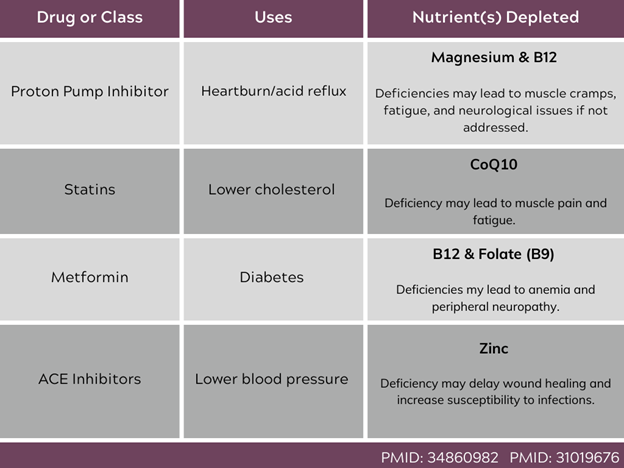
Drug-Induced Nutrient Depletions (DIND) occur when certain medications cause the body to lose or use up essential nutrients. Unfortunately, these depletions often go unnoticed when medications are prescribed. Here are a few common examples highlighted in the table below. These examples call attention to the need to monitor nutritional status and for clinicians to suggest appropriate supplements when necessary.
Table 1: Examples of DINDs of commonly prescribed medications
Examples of common Drug–Induced Nutrient Depletions of commonly prescribed medications
Key Drug-Nutrient Interactions (DNI)
Drug-Nutrient Interactions (DNI) happen when a drug and a nutrient affect each other in the body. Despite their potential impact, DNIs are often not a part of the conversation around prescription drugs. However, studies have shown that as many as 48% of patients taking prescription drugs have been found to be at risk for a DNI. These interactions can alter how the drug or nutrient is absorbed, distributed, metabolized, or excreted. Some examples include:
- Fatty foods can increase the absorption of some lipid-soluble drugs, such as certain antipsychotics and antiepileptics, potentially leading to higher than expected drug levels and increased side effects.
- Antibiotics can alter the gut microbiome and lead to vitamin K deficiency, which is crucial for blood clotting. This interaction is particularly significant for individuals on anticoagulant therapy, as it can lead to an increased risk of bleeding.
- Grapefruit inhibits the CYP3A4 enzyme – a detoxification enzyme needed to metabolize certain statins, calcium channel blockers, and immunosuppressants. Recognizing these food-drug interactions allows clinicians to counsel patients effectively, preventing potentially dangerous drug toxicity in individuals taking medications that rely on this enzyme for metabolism.
- Certain nutrients (like iron or calcium) can form insoluble complexes with medications, such as tetracycline and fluoroquinolones antibiotics or bisphosphonates (i.e. alendronate), reducing their bioavailability and effectiveness. Individuals are often advised to take these medications at different times from their supplements to avoid this issue.
Understanding these interactions allows clinicians to tailor interventions that minimize risks and enhance the therapeutic efficacy of both medication and supplement.
Managing Drug-Herb Interactions (DHI)
Drug-Herb Interactions occur when prescription medications and herbal supplements are used together. These can change the effectiveness or safety of the drug. For instance, St. John’s Wort can interact with many medications, such as antihypertensives, oral contraceptives, and certain antidepressants, potentially leading to reduced drug effectiveness or increased side effects.
- John’s Wort induces the activity of the CYP3A4 enzyme, which can lead to decreased levels of medications metabolized by this pathway, reducing their efficacy. This includes drugs like cyclosporine, used in organ transplant patients, and certain antiretrovirals used in HIV treatment.
- Ginkgo Biloba, often used for cognitive enhancement, can increase the risk of bleeding when taken with anticoagulants like warfarin or antiplatelet drugs like aspirin.
- Echinacea, commonly used to prevent colds, can interact with immunosuppressants, potentially reducing their effectiveness and compromising the management of autoimmune diseases or organ transplant patients.
Healthcare professionals need to be aware of and careful when dealing with drug-herb interactions (DHIs). They should know how herbal products work in the body and how they might interact with prescription medicines.
At the same time, we want to be careful not to be overly cautious and prevent safe and potentially beneficial use of herbs alongside medications. By giving good advice on safe herb-drug combinations, clinicians can gain the trust of patients and can help prevent harmful side effects while simultaneously improving treatment results.
The Importance of Research and Personalized Care in Drug-Nutrient Interactions
One of the challenges in the field of nutrient-depletions is the lack of robust research data. Most evidence comes from lab studies or animal models, with limited human clinical trials. However, understanding these interactions is crucial for providing informed and personalized healthcare. By integrating knowledge of DNIs, DINDs, and DHIs, healthcare professionals can offer personalized lifestyle advice and improve drug prescribing practices.
The personalized care approach includes:
- Regular Monitoring: Routine checks of nutrient levels in patients on long-term medications that are known to cause nutrient depletions.
- Patient Education: Informing patients about potential interactions and how to manage them, including dietary adjustments and timing of supplement intake.
- Collaborative Care: Working in a team of healthcare providers, including pharmacists, doctors, and nutritionists, to ensure a holistic approach to patient care.
Conclusion and final thoughts
As interest in a holistic approach to health grows among consumers and patients, understanding the interactions between drugs, nutrients, and herbs becomes more important for clinicians. Health professionals—including physicians, pharmacists, nutritionists, and other allied health professionals—can work together to provide comprehensive and personalized care.
Fellow clinicians, by staying informed and seeking unbiased education about these interactions, we can help individuals use nutraceuticals safely and effectively. This collaborative approach not only enhances patient safety, but also fosters a more holistic approach to healthcare.
References
- Lordan R. Dietary supplements and nutraceuticals market growth during the coronavirus pandemic – Implications for consumers and regulatory oversight. PharmaNutrition. 2021;18:100282. doi:10.1016/j.phanu.2021.100282.
- Djaoudene O, Romano A, Bradai YD, et al. A Global Overview of Dietary Supplements: Regulation, Market Trends, Usage during the COVID-19 Pandemic, and Health Effects. Nutrients. 2023;15(15):3320. Published 2023 Jul 26. doi:10.3390/nu15153320
- Prescott JD, Drake VJ, Stevens JF. Medications and Micronutrients: Identifying Clinically Relevant Interactions and Addressing Nutritional Needs. J Pharm Technol. 2018;34(5):216-230. doi:1
- Jaynes M, Kumar AB. The risks of long-term use of proton pump inhibitors: a critical review. Ther Adv Drug Saf. 2018;10:2042098618809927. Published 2018 Nov 19. doi:10.1177/20420986188099270.1177/8755122518780742
- Amadi CN, Mgbahurike AA. Selected Food/Herb-Drug Interactions: Mechanisms and Clinical Relevance. Am J Ther. 2018;25(4)
. doi:10.1097/MJT.0000000000000705. - Cleveland Clinic. Bisphosphonates. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/24753-bisphosphonates. Published December 6, 2022. Accessed July 9, 2024.
- Hogle BC, Guan X, Folan MM, Xie W. PXR as a mediator of herb-drug interaction. J Food Drug Anal. 2018;26(2S)
. doi:10.1016/j.jfda.2017.11.007. - Fasinu PS, Bouic PJ, Rosenkranz B. An overview of the evidence and mechanisms of herb-drug interactions. Front Pharmacol. 2012;3:69. Published 2012 Apr 30. doi:10.3389/fphar.2012.00069.
- Pan HY, Wu LW, Wang PC, Chiu PH, Wang MT. Real-world Evidence of the Herb-drug Interactions. J Food Drug Anal. 2022;30(3):316-330. Published 2022 Sep 15. doi:10.38212/2224-6614.3428.
- Karadima V, Kraniotou C, Bellos G, Tsangaris GT. Drug-micronutrient interactions: food for thought and thought for action. EPMA J. 2016;7(1):10. Published 2016 May 12. doi:10.1186/s13167-016-0059-1.
You May Also Like...
Basic Nutrition 101
Basic Nutrition 101 Probably one of the most common questions I get as a nutritionist is, “what should I be eating?”…
Healthy Hair, Skin, and Nails
Healthy Hair, Skin, and Nails: A Nutritional Approach The condition of your hair, skin, and nails (AKA the…
Stay In Touch!
Join my mailing list to keep up with all the latest nutrition & FxMed learning opportunities



