The gut microbiome plays a much larger role in hormone regulation than most people realize. While its influence on digestion and immunity is well known, certain gut bacteria also directly impact how the body processes and eliminates estrogen.
Comprehensive patient care for anyone dealing with symptoms related to hormonal dysregulation (such as PMS/PMDD, headaches, PCOS, endometriosis) or taking an oral contraceptive or hormone replacement therapy (HRT) must not overlook this critical connection.
The Microbiome & Estrogen: A Critical Relationship
Estrogen is produced in the ovaries, fat tissue, and adrenal glands, but it doesn’t simply disappear after use. Once the body has used it, estrogen must be metabolized, detoxified, and excreted through the liver and gut. If this system is not functioning efficiently, estrogen can be reabsorbed, leading to hormone imbalances, worsened PMS, bloating, and inflammation.
One of the most important players in this process is a specific subset of gut bacteria known as the estrobolome.
What is the Estrobolome?
The estrobolome is a collection of gut bacteria that regulate estrogen metabolism and clearance. These microbes produce the enzyme beta-glucuronidase, which plays a critical role in determining whether estrogen is eliminated or recirculated in the body.
When the estrobolome is balanced, it helps remove excess estrogen efficiently, preventing hormonal imbalances.
When it’s dysregulated, estrogen that was supposed to be excreted can be reactivated and reabsorbed, increasing the risk of estrogen dominance, PMS, and hormone-related symptoms like bloating, headaches, and heavy periods.
Factors That Disrupt the Estrobolome
A well-functioning estrobolome is essential for maintaining hormone balance, but several factors can throw this system off track.
- Gut Dysbiosis – Overgrowth of certain bacteria can lead to excess beta-glucuronidase activity, which causes estrogen to be reabsorbed instead of eliminated.
- Chronic Constipation – The longer stool sits in the colon, the higher the chance that estrogen will be reabsorbed rather than excreted.
- Low-Fiber Diets – Fiber binds to estrogen in the gut, helping to escort it out of the body. Without enough fiber, this process is less efficient.
- Inflammation & Leaky Gut – A damaged intestinal lining makes it easier for inflammatory compounds to disrupt estrogen metabolism.
- Antibiotic Use – Broad-spectrum antibiotics can wipe out beneficial bacteria involved in estrogen clearance, creating long-term imbalances.
Oral contraceptives (OCs) can also influence the estrobolome. Research indicates that OC use may lead to alterations in the gut microbiome, including changes in bacterial diversity and function. These alterations can disrupt the estrobolome’s ability to regulate estrogen metabolism effectively.
Additionally, OCs have been associated with nutrient depletions—such as vitamins B, C, and E, as well as minerals like zinc and magnesium—that are vital for maintaining gut health and supporting the enzymes involved in estrogen detoxification. As a result, OC use may contribute to hormonal imbalances and symptoms of to impaired estrogen metabolism.
Read more about drug-induced nutrient depletions (DIND) associated with OCPs here.
The Liver’s Role in Estrogen Detoxification
The liver plays a central role in estrogen metabolism, ensuring that once estrogen has done its job, it is safely processed and eliminated. This occurs in two distinct but interconnected detoxification phases.
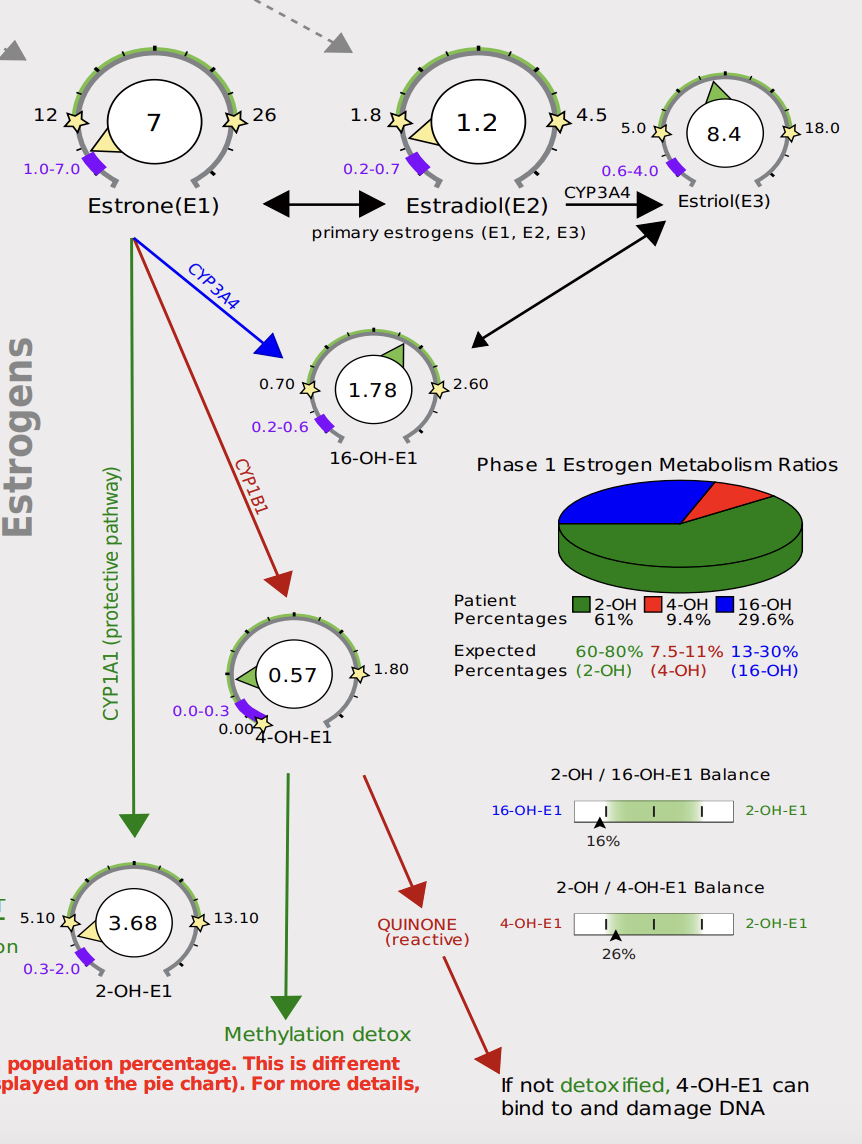
Phase 1: Estrogen Metabolism via Cytochrome P450 Enzymes
In this initial step, the liver uses cytochrome P450 enzymes to convert estrogen into hydroxylated metabolites—primarily 2-hydroxyestrone (2-OH), 4-hydroxyestrone (4-OH), and 16-hydroxyestrone (16-OH). These metabolites vary in their biological activity:
- 2-OH is the most protective form and is more easily cleared.
- 4-OH and 16-OH are more reactive and have been associated with increased estrogenic activity and DNA damage if not properly detoxified.
This phase requires key nutrients like B vitamins (B2, B6, B12, folate), magnesium, and glutathione to function efficiently.
Phase 2: Estrogen Conjugation & Clearance
Once estrogen has been metabolized, Phase 2 detoxification prepares it for elimination by conjugating (binding) it to molecules like glucuronide and sulfate, making it water-soluble and ready for excretion. This step occurs through the following pathways:
- Glucuronidation – Uses calcium-D-glucarate to bind estrogen for excretion through bile and stool.
- Sulfation – Attaches sulfate molecules, aided by sulfur-rich foods like garlic, onions, and cruciferous vegetables.
- Methylation – A critical step regulated by SAMe, magnesium, and methyl donors (B12, folate), converting estrogen metabolites into a form the body can efficiently remove.
What Happens When Liver Detoxification is Impaired?
If either phase is compromised due to nutrient deficiencies, poor bile flow, high toxin exposure, or sluggish digestion, estrogen metabolism slows down. This can lead to:
- Recirculation of estrogen rather than proper elimination, contributing to estrogen dominance.
- An accumulation of reactive estrogen metabolites may increase inflammation and oxidative stress.
- Symptoms like bloating, PMS, heavy periods, and hormone-related headaches.
Because the liver and gut work together, any dysfunction in one impacts the other. Supporting both liver detoxification and gut health is critical for maintaining hormonal balance and optimizing estrogen metabolism.
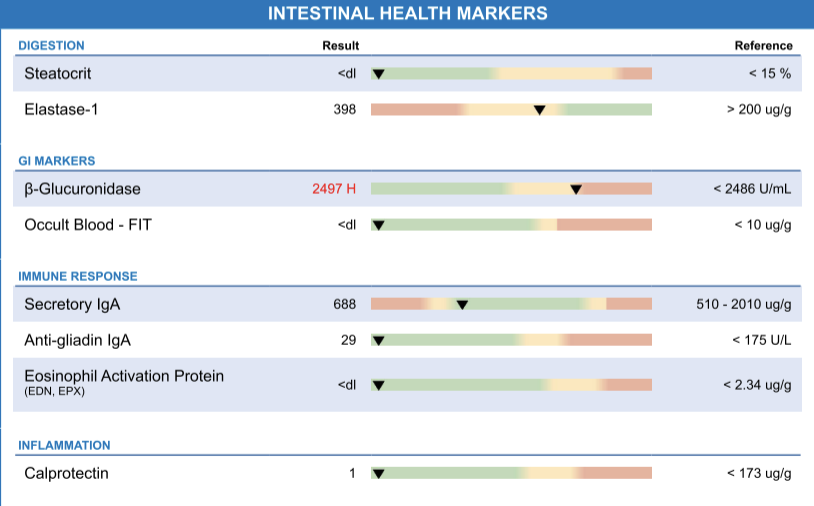
Key Gut Markers for Assessing Estrobolome Function
Functional stool testing can provide insights into how well the estrobolome is functioning and whether estrogen metabolism is being disrupted.
- Beta-Glucuronidase Levels – Elevated levels indicate that estrogen is being reabsorbed, which may contribute to estrogen dominance.
- SCFA (Short-Chain Fatty Acids) Production – SCFAs like butyrate support gut barrier integrity and help regulate inflammation, which influences estrogen metabolism.
- Microbiome Diversity – A lack of diversity in gut bacteria is linked to hormonal imbalances and poor estrogen clearance.
- Inflammation Markers (Calprotectin, Zonulin) – Increased gut permeability may contribute to poor estrogen metabolism and histamine overload.
HRT, Oral Contraceptives & the Estrobolome
Hormone replacement therapy (HRT) and oral contraceptives (OCPs) introduce exogenous estrogen into the body. Because the estrobolome helps metabolize and regulate estrogen, gut health can directly impact how the body processes these hormones.
Disruptions in gut bacteria may cause variability in how individuals respond to HRT or birth control, leading to bloating, nausea, mood swings, or breakthrough bleeding. Maintaining a healthy microbiome can enhance hormone therapy outcomes and minimize unwanted side effects.
Dietary Strategies to Support the Estrobolome
What you eat directly impacts how efficiently estrogen is metabolized and eliminated. Key dietary strategies include:
- Cruciferous Vegetables (Broccoli, Kale, Cauliflower) – Provide sulforaphane, which supports estrogen detoxification pathways.
- Flaxseeds & Chia Seeds – Contain fiber and phytoestrogens that help bind and regulate estrogen levels.
- Healthy Fats (Olive Oil, Avocado, Nuts) – Support gut barrier function and bile production.
- Polyphenol-Rich Foods (Berries, Pomegranate, Green Tea) – Help feed beneficial gut bacteria involved in estrogen metabolism.
- Adequate Hydration & Electrolytes – Essential for proper bile flow and toxin elimination.
While these dietary strategies provide a strong foundation for supporting the estrobolome, they should be personalized based on individual hormone patterns and estrogen-related conditions:
- Estrogen Dominance (High Estrogen, Low Progesterone) – Focus on fiber-rich foods, cruciferous vegetables, and calcium-D-glucarate to enhance estrogen clearance and reduce reabsorption.
- PCOS & Androgen-Dominant Patterns – Balance insulin levels with steady blood sugar support (protein, healthy fats, fiber) while optimizing liver function to promote healthy estrogen-androgen ratios.
- Perimenopause (Fluctuating Estrogen, Lower Progesterone) – Support hormone metabolism with phytoestrogen-rich foods like flaxseeds, along with liver and gut-friendly nutrients to help stabilize shifting hormone levels.
Each stage of hormone health presents unique challenges, and fine-tuning diet and lifestyle strategies to match individual needs can make a significant impact.
Nutraceuticals for Supporting the Estrobolome
In addition to dietary strategies, specific nutraceuticals can support estrogen metabolism and gut health by influencing detoxification pathways, microbiome balance, and hormone regulation. The following are some evidence-based examples; this is by no means is this an exhaustive list:
- Calcium-D-Glucarate – Helps eliminate excess estrogen by inhibiting beta-glucuronidase, an enzyme that can otherwise lead to estrogen reabsorption.
- Diindolylmethane (DIM) & Indole-3-Carbinol (I3C) – Both derived from cruciferous vegetables, these compounds support healthy estrogen metabolism. DIM is often preferred due to its stability and bioavailability.
- Maca Root – An adaptogen known for supporting hormone balance, particularly in perimenopause and menstrual cycle regulation.
- Vitex (Chaste Tree Berry) – Helps regulate menstrual cycles and progesterone levels, making it useful for PMS and cycle-related symptoms.
- Probiotics (Bifidobacterium Longum, Lactobacillus Rhamnosus GG) – Support gut health and estrogen metabolism while reducing inflammation and histamine-related symptoms.
- Prebiotics (Inulin, FOS) – Feed beneficial gut bacteria, promoting a balanced microbiome to support hormone regulation.
- Sulforaphane (Broccoli Sprout Extract) – Enhances liver detoxification, improving the clearance of estrogen metabolites.
- Resveratrol & Curcumin – Help regulate gut inflammation and support microbiome diversity, which impacts estrogen balance.
- Magnesium (Glycinate, Citrate) – Supports hormone metabolism, gut motility, and bile flow. Magnesium glycinate is best for overall hormone support, while magnesium citrate may help with constipation and estrogen clearance.
A Personalized Approach is Key
The best supplement strategy depends on individual hormone imbalances.
- Estrogen Dominance – DIM, calcium-D-glucarate, and fiber to promote estrogen clearance.
- PCOS & Androgen-Dominance – Insulin-supportive nutrients, probiotics, and liver detox support.
- Perimenopause & Estrogen Fluctuations – Maca, Vitex, and adaptogenic herbs for hormone modulation.
Since gut health, liver function, and hormone balance are highly individualized, it’s essential to work with a clinician who can personalize and guide supplement choices based on your unique needs.
Final Thoughts
Understanding the estrobolome is a crucial piece of the hormone health puzzle. Addressing gut imbalances, optimizing liver detoxification, and implementing targeted diet and supplement strategies can support estrogen metabolism, reduce symptoms of estrogen dominance, and promote overall well-being.
References
- Kumari N, Kumari R, Dua A, et al. From gut to hormones: unraveling the role of gut microbiota in (phyto)estrogen modulation in health and disease. Mol Nutr Food Res. 2024; e2300688. doi:10.1002/mnfr.202300688.
- Salliss M, Farland L, Mahnert N, Herbst-Kralovetz M. The role of gut and genital microbiota and the estrobolome in endometriosis, infertility, and chronic pelvic pain. Hum Reprod Update. 2021. doi:10.1093/humupd/dmab035.
- Prabakar S, K M, M K, et al. Automated liver detox therapy. 2024 2nd International Conference on Artificial Intelligence and Machine Learning Applications Theme: Healthcare and Internet of Things (AIMLA). 2024;1-7. doi:10.1109/AIMLA59606.2024.10531483.
- Hu S, Ding Q, Zhang W, et al. Gut microbial beta-glucuronidase: a vital regulator in female estrogen metabolism. Gut Microbes. 2023;15. doi:10.1080/19490976.2023.2236749.
- Honda S, Tominaga Y, Espadaler-Mazo J, et al. Supplementation with a probiotic formula having β-glucuronidase activity modulates serum estrogen levels in healthy peri- and postmenopausal women. J Med Food. 2024. doi:10.1089/jmf.2023.k.0320.
- Della Torre S. Non-alcoholic fatty liver disease as a canonical example of metabolic inflammatory-based liver disease showing a sex-specific prevalence: relevance of estrogen signaling. Front Endocrinol (Lausanne). 2020;11. doi:10.3389/fendo.2020.572490.
- Ayyadurai V, Vajro P, Colecchia A. Mechanistic understanding of D-glucaric acid for liver detoxification. Mol Nutr Food Res. 2023. doi:10.1002/mnfr.202300123.
- Williams DE. Indoles and cancer chemoprevention. Mol Nutr Food Res. 2021;65(1):e2000149. doi:10.1002/mnfr.202000149.
- Odimegwu DC, Oyinkansola OA. Qualitative analysis of cruciferous vegetable extracts for DIM. Food Chem. 2023;370:131055. doi:10.1016/j.foodchem.2021.131055.
- Makris G, Trifonidi E, et al. Effect of supplementation with prebiotics on levels of gut microbiota and vitamin absorption. Nutrients. 2024;16(2):349. doi:10.3390/nu16020349.
- Wong RHX, Zaw T, et al. Regular supplementation with resveratrol improves bone mineral density and hormonal balance. Nutrients. 2020;12(3):761. doi:10.3390/nu12030761.
- Drăgoi CM. Potent NRF2-activating dietary supplements: potential in hormonal and gut health. J Funct Foods. 2020;65:103738. doi:10.1016/j.jff.2019.103738.
- Capozzi A, Scambia G, et al. Calcium, vitamin D, vitamin K2, and magnesium supplementation and skeletal health: a review. J Endocrinol Metab. 2020;10(1):27-33. doi:10.14740/jem625.
- Hong T, Zou J, Jiang X, et al. Curcumin supplementation ameliorates bile cholesterol supersaturation in hamsters by modulating gut microbiota and cholesterol absorption. Nutrients. 2022;14(9):1828. doi:10.3390/nu14091828.
- Feng D, Jiang X, Hong T, et al. Hepatoprotective effect of curcumin against bisphenol A-induced hepatic steatosis via modulating gut microbiota dysbiosis and related gut-liver axis activation in CD-1 mice. J Nutr Biochem. 2022;109:109103. doi:10.1016/j.jnutbio.2022.109103.
- Del Carpio N, Alvarado-Corella D, Quiñones-Laveriano D, et al. Exploring the chemical and pharmacological variability of Lepidium meyenii: a comprehensive review of the effects of maca. Front Pharmacol. 2024;15:1360422. doi:10.3389/fphar.2024.1360422.
- Bizinelli D, Navarro F, Faldoni F. Maca root (Lepidium meyenii) extract increases the expression of MMP-1 and stimulates migration of triple-negative breast cancer cells. Nutr Cancer. 2021;74(2):346-356. doi:10.1080/01635581.2021.1882511.
You May Also Like...
Optimizing Thyroid Function
Optimizing Thyroid Function It might be tiny, but thyroid gland is powerful! According to the American Thyroid…
Reduce Food waste & Save Money
Reduce Food waste & Save Money Why reduce food waste? Did you know that each day, Americans toss out enough food to…
Stay In Touch!
Join my mailing list to keep up with all the latest nutrition & FxMed learning opportunities



